1 Make the complex simple
2 Value the importance of governance
3 Address operational needs with intense discipline
1 Make the co mplex simple
mplex simple
The solution blueprint for Singapore’s NEHR included a framework for sophisticated business logic, analytics, decision support and other services. For the initial phase, however, Singapore focused on “Continuity of Care”. The requirements for achieving this initial vision: a rich, view-only system with clinical events, investigation reports, radiology reports, alerts and allergies, immunization records, medications and a host of supporting documents (such as discharge summaries and emergency department notes).
The project is led by MOH Holdings (MOHH), the holding company of Singapore’s public healthcare assets. Over the long term, MOHH plans to incorporate new capabilities into the system. But in the short term, the organization opted to think big but start simple. This approach enabled the project team to address three fundamental challenges:
I. Managing data from multiple sources.
Bringing together the various data sources across Singapore introduced a host of complexities around data codification and standards. Because of the number and diversity of healthcare organizations and their clinical systems, there were significant variations across the data. Some data were coded (using medical coding to denote specific diagnoses or procedures); and some were uncoded (using narrative or free-form descriptions instead of a set of widely agreed upon codes). Similarly, some data and documents were highly structured, while others were unstructured, offering only large chunks of text. Some data items were well populated by one organization, but poorly populated by another.
 The team also encountered different definitions of basic concepts, such as “movement”, “visit”, “event” and “episode”. Mapping multiple hospitals’ approaches to a common data model proved an important challenge—one the team had to overcome before it could address more sophisticated analytics and decision support objectives.
The team also encountered different definitions of basic concepts, such as “movement”, “visit”, “event” and “episode”. Mapping multiple hospitals’ approaches to a common data model proved an important challenge—one the team had to overcome before it could address more sophisticated analytics and decision support objectives.
A deep dive of the actual production data from source systems uncovered many of the subtleties in codification, structure, availability and meaning. This drove the design team to focus on making use of the as-is data, rather than what the data could potentially be. The rational was that a system which interprets data or provides derived data could introduce clinical risks if the underlying data had gaps or differences in meaning.
Thus, the complexity of disparate data from multiple sources was overcome by the use of production data analysis and the decision to focus on raw data for the initial release.
II. Engaging clinicians.
By using screen mock-ups of the NEHR in clinician workshops, the team in Singapore was able to identify which features and functionalities appealed to end users. The project team engaged clinicians as early as possible in the process, in order to understand their preferences and help drive towards a simpler and more intuitive interface.
III. Addressing functional, technical and operational implications.
Besides engaging clinicians, the project team integrated the discussion of functional, technical and operational issues and concerns from the very beginning. The functional, technical and operational teams all helped to shape the final solution design decisions.
An integrated approach helped to ensure that the functionality and data could be supported operationally and technically. Quite simply, the solution had to work: it had to be able to meet service level agreements, and it had to be maintainable in a way that was feasible and pragmatic.
SINGAPORE’S VISION To improve healthcare quality for all residents, increase patient safety, lower healthcare costs and develop more effective health policies, Singapore’s MOH created the NEHR vision – “One Singaporean, One Health Record” – which enables patient health records to be shared across the nation’s healthcare ecosystem. THE HEALTHCARE ECOSYSTEM IN SINGAPORE The health ecosystem in Singapore has about 5.1 million residents and more than 36,000 healthcare providers across the public and private sectors. Private practitioners provide 80 percent of primary healthcare services, and the government polyclinics provide the balance. The ratio changes for more costly hospital care, with the government providing 80 percent through eight public hospitals. |
2 Value the importance of governance
In a perfect world, all data sources would provide uniform and quality data. Of course, the real world is far more complicated. With that in mind, it was important to focus on understanding up front what was available and work within those confines to aggregate data without losing meaning. The work in Singapore also underscored the importance of governance in bringing together organizations and systems. Three types of governance were put in place:
I. Technical Solution—including Architecture, Security and Operations
II. Clinical Solution—including Usability, User Functionality and clinical risk
III. Information governance—including Data Standards and Data Quality
 The work in Singapore reinforced the need for specific activities and assets to support effective governance. Regional or national EHRs need formal data-sharing agreements that provide a legal framework for defining the responsibilities of the participating entities. In Singapore, where many of the organizations, systems and sources of data fall under the same government, such agreements were relatively simple to achieve. In other jurisdictions, where public and private-sector heath organizations intersect, these agreements would likely be more complex and much more critical.
The work in Singapore reinforced the need for specific activities and assets to support effective governance. Regional or national EHRs need formal data-sharing agreements that provide a legal framework for defining the responsibilities of the participating entities. In Singapore, where many of the organizations, systems and sources of data fall under the same government, such agreements were relatively simple to achieve. In other jurisdictions, where public and private-sector heath organizations intersect, these agreements would likely be more complex and much more critical.
Another important area was policy—including privacy policies, patient enrollment, and data sensitivity considerations. These policies had to be addressed early in the process, as the decisions would affect solution design.
MOHH and Accenture also designed the Singapore architecture to be inherently flexible—making it easier to implement changes as policies evolves over time.
NEHR FIRST STEPS: UNIFYING CLINICIANS’ VIEW OF PATIENT DATA In April 2011, MOHH completed the first release of its EHR implementation. The EHR has these capabilities: 1. A national Health Identification Service (NHIS). The NHIS is a patient master index that enables the EHR to match patient records received from across the health domain in Singapore. It enables users to uniquely identify people through a combination of factors—including the national identifier, name, date of birth, address and other demographic information. 2. Summary care record. The NEHR delivers a summary care record for each patient. A summary care record provides a concise overview of the most recent clinical activities of an individual. These can include recent laboratory results, medications and the most recent health events—in other words, a highlevel overview of the patient’s health. From here, clinicians can navigate to more detailed data and documents. 3. Access to Discharge and Event Summaries. These documents provide high-level overviews of specific clinical episodes (such as hospital admissions). 4. Access to Health Data in national registries. Singapore’s NEHR also serves as a doorway to accessing health data residing in existing national registries for immunization, medical alerts and allergies. This capability also leverages Singapore’s Electronic Medical Record Exchange (EMRX) system to enable access to older clinical documents. 5. Privacy and Security. Privacy and security are critical to the NEHR. In Singapore, the system incorporates role-based access, data sensitivity classification, as well as “break-the-glass” functionality (which enables clinicians to access patient information outside of normal security and privacy settings if needed in an emergency). 6. Audit and logging capability. The Singapore system includes full audit logging capabilities—capturing who has accessed the information, when, where and how. |
3 Address operational needs with intense discipline
From the beginning, MOHH and the project team took a disciplined approach to security operations, technical operations and service management. In addition, operational areas specific to an EHR were defined. These included:
I. User provisioning and developing clear procedures for granting role-based access to the system
II. Ongoing data integration operations
– Investigation of message failures or data discrepancies
– Synchronization of data patching between the data sources and the national EHR
– Synchronization and ongoing management of code sets between the data sources and the national EHR
The project also underscored the importance of the following:
III. Change coordination and management across different systems
It was critical to understand the plans for source system upgrades and enhancements, as these changes could have significant impact on the EHR system.
IV. Ongoing analysis of production data
This was performed for historical data load and in the initial stages of message integration and was key to anticipating the types and frequency of errors, and the possible risks.
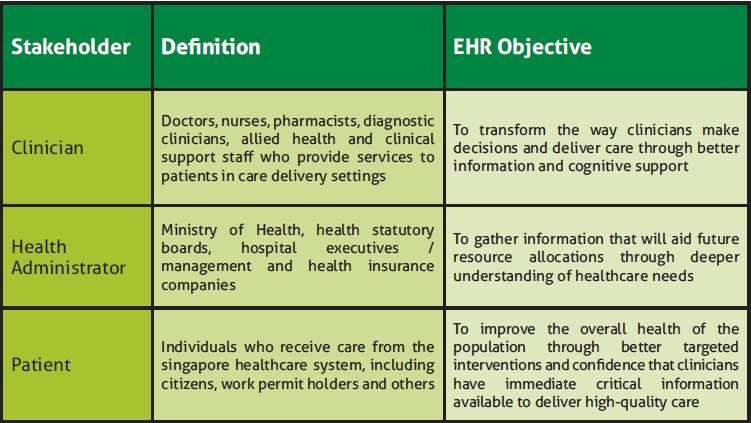
NEHR ARCHITECTURE: STARTING WITH THE END IN MIND Working with Accenture, MOHH invested in the development of a goal-state architecture. This architecture serves as the blueprint for achieving the short-term and longterm goals of the NEHR and for addressing the needs and goals of three core stakeholders (see Figure 1). At a high level, the blueprint includes four core elements:
2. Data Sources, including clinical and supporting systems, which provide patient and clinical data through the nationwide EHR. In Singapore, the primary sources are the public hospitals’ and polyclinics’ EMR systems, registration systems and ancillary systems. National registries also provide data to the EHR. 3. EHR Information Exchange, which is a set of services and repositories to facilitate the sharing of information. Singapore’s solution relies on an enterprise service bus to enable the exchange of patient and clinical information among the nationwide EHR system, the data sources and the data consumers. The architecture is designed to enable the nationwide EHR to be a producer, consumer and supplier of data. 4. Technology infrastructure, which provides the supporting platforms, integration, security and operations capabilities. |
Into the future
Achieving Singapore’s goal to build and deploy a robust NEHR is an ongoing process that began with the country’s “One Singaporean, One Health Record” vision where patients are able to move seamlessly within an integrated care system. Despite its challenges, the journey stands as an example of efforts that can be made to improve quality of care and health outcomes while optimizing efficiency and cost.