Researchers from the Netherlands Cancer Institute and others have shown that it is possible to obtain immune cells (so-called killer T cells) from the bloodstream of a cancer patient and expand them in a dish together with a living piece of tumor from the same patient.
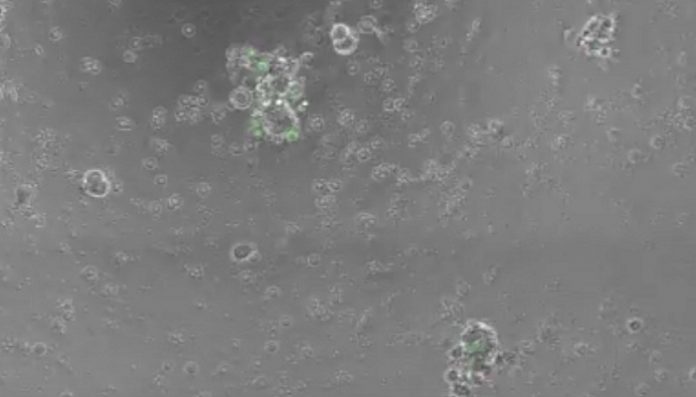
Such a tumor piece is called a tumor organoid. The immune cells develop the ability to kill the tumor cells and to reduce organoid size, while leaving healthy control tissue of the same patient untouched.
This gives research into immunotherapy an instrument with which, for an individual patient — but outside the body — the complex interaction between immune cells and cancer cells can be studied. The researchers will also use this new research platform to enable – in the long term – cellular immunotherapy: treatment of the patient with his or her own immune cells as ‘living drugs.’
Researchers Krijn Dijkstra, Chiara Cattaneo et al. will publish these results on Thursday August 9th on the website of the scientific journal Cell. The research was led by Emile Voest (contact person) and Ton Schumacher.
Tumor organoids retain properties of tumor
Recently, tumor organoids have been shown to retain the morphological and mutational properties of the original tumor. This has opened the door to studying tumors outside the patient’s body and to testing the effects of various drugs. However, tumor organoids had not yet been used to study immunotherapy. Now, that has become possible.
Krijn Dijkstra, physician-researcher who is writing his doctoral thesis on this study: ‘to answer our questions about whether or not immune therapy is successful, there is a great need for good “real life” models. This is certainly going to help.’
We were anxiously waiting for such a research platform,’ says internist-oncologist Emile Voest, who has led the research. ‘And there are no laboratory animals involved.’
Why does one patient respond while another does not?
This new tumour model allows researchers to more easily study the big questions and bottlenecks that now frustrate the wide clinical application of immunotherapy. For example: why does one patient respond well to immunotherapy and another not at all? How do cancer cells bypass the immune system and how do immune cells react to that? And finally: how can we intervene in all these mechanisms?
Colorectal cancer and lung cancer
The organoids were cultured from tumor tissue from 13 patients with a specific form of colorectal cancer (mismatch repair deficient colorectal cancer) and 6 patients with non-small cell lung cancer. These subtypes of cancer are partly sensitive to immunotherapy, because the amount of DNA damage is so substantial that the immune system recognizes the cancer cells as ‘foreign’. However, only a minority of patients with metastatic cancer responds well to immunotherapy. Using organoids, immune cells from the blood of about one in three patients were successfully ‘trained’ to recognize tumor cells.
T cells recognize and kill tumor cells
The immune cells in question are T cells. T cells (for the expert: type CD8+) are white blood cells with a dual function: they recognize foreign elements and kill them as well, hence the nickname killer T cells. From the bloodstream, they infiltrate and attack the tumor. In the forms of immunotherapy that are now used – as standard treatment or experimentally – these T cells take the front stage. However, in the micro-environment of the tumor, all kinds of mechanisms are at work that make it impossible, or no longer possible, for T cells to recognize or kill the cancer cells. These mechanisms can now be studied better.
‘Fresh T cells’
Immunotherapy is aimed at strengthening and/or expanding T cells in the tumor microenvironment. Immunotherapy was first applied to cutaneous melanoma, an aggressive form of skin cancer, and only afterwards to several other cancers. ‘With melanoma, it is relatively easy to grow T cells from the tumor itself,’ says Voest. ‘That has proved much more difficult with epithelial cancers such as colorectal cancer and lung cancer.’ That is why he is so happy that his group has succeeded in obtaining T cells from the bloodstream. ‘T cells from the bloodstream are also likely to be ‘fresher’ than T cells that have already become exhausted during their stay in the tumor microenvironment.’
The new discovery also opens the way to develop cellular therapy in which T cells are ‘trained’ outside the body to recognize the tumor and then returned to the patient. The organoids can likewise be used to test combinations of immunotherapy and other therapies.
About the Netherlands Cancer Institute
The Netherlands Cancer Institute is at the international forefront of cancer care and research for already more than a century. The unique combination of health care and scientific research within the same institute offers great benefit for cancer patients. Specialized cancer care professionals work together in multidisciplinary teams every day to set up and carry out treatment plans tailored to the needs of individual patients because no two tumors are alike. Cancer patients or people suspected of having cancer can come to our hospital, known as the Antoni van Leeuwenhoek, to make use of this personal approach and the state-of-the-art research and treatment facilities. The research institute employs more than 650 scientists investigating many aspects of cancer development, diagnosis, treatment and epidemiology. Scientists at the Netherlands Cancer Institute have access to state-of-the-art research facilities supporting their basic, translational and clinical research.
This scientific research could not be carried out without the institutional support of the Dutch Cancer Society, the Ministry of Health, Welfare and Sport, the many research grants obtained by our researchers from (inter)national funding agencies, and the generous donations made by individuals that support our research program. The Netherlands Cancer Institute is the only OECI designated Comprehensive Cancer Center in the Netherlands. For more information please visit our websites www.nki.nl and www.avl.nl