Health is a top priority globally, and healthcare is considered crucial for sustainable development. In the recently released Sustainable Development Goals – SDGs (‘17 Goals to Transform Our World in United Nations, 2015’), ‘Good Health & Well-Being’ is one of the top three goals. Especially in developing countries like India, healthcare remains a priority, considering that India is the second populous country in the world with a current population of 1.31 billion(WHO, 2017).
This implies that India has a long way to go to address the healthcare needs of its ever-growing population.
Despite focus on healthcare as a top priority across nations, healthcare spending remains a challenge. This aspect has created a wide disparity among nations with respect to the quality of treatment and patient experience during their stay in hospital for long-term care.
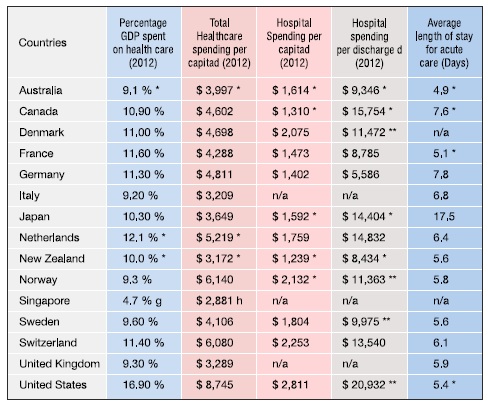
In developed nations such as the United States, investment in health care approximates to US$ 3.0 trillion, and accounts for 17.5 Percent of the Gross Domestic Product (GDP) (reference, 2014). It means that USA alone spends one out of five dollars on health (the per capita health care spending was US$ 9523 (reference, 2014). Specifically, the hospital spending in USA increased to US$ 971.8 billion. This amount is about one-third of the total healthcare spending of United States (Centre for Medicare & Medicaid Services, USA, 2015), and as per some experts, hospital cost is a major expenditure in USA (Halvorson, 2009 p. 135). It’s not just the USA, but the trend for hospital costs is similar across many developed nations as illustrated in table below.
Hospital Costs versus the total healthcare expenditure across developed nations
- The Data quoted above is for 2012 unless noted
- * 2011. **2012. ***2002-2011. *1. Adjusted for difference in the cost of living PPP, purchasing power parity adjustment).
- Adjusted for difference in the cost of living (PPP; purchasing power parity adjustment).
- Source: World Bank, 2014
- Source; World Bank , 2014:2005 purchasing power parity (ppp) adjustment
Similarly, for Malaysia, in 2009, of the total expenditure on health by provider (Public and Private) of health services; 54.1 percent went to hospitals (Asia Pacific Observatory on Health Systems and Policies, 2012).
An analysis of the per capita expenditure per day gives an alarming picture of spending by Indian population – ranging from poor to high-income earners.
Expenditure based on socio-economic status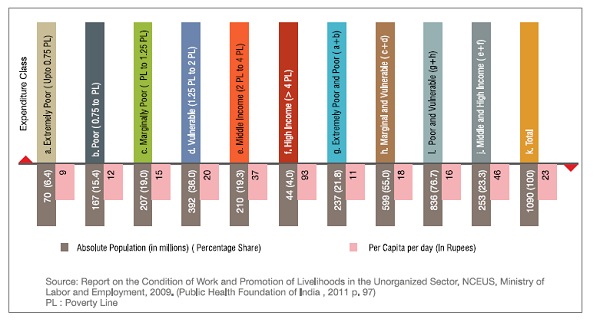
About 10 percent of Indian households spend a large share of their income on health care (Jha, et al., 2009).
Studies have reported that about 2.1 million residents of India get pushed into poverty due to medical costs, 24 percent of all the IPD patients and 40 percent of all the patients borrow money to meet the healthcare expenses, making healthcare as the second most important cause of rural debt. (Mishra, 2013). It is estimated that 3.3 % of India’s population gets impoverished due to illness every year. Poorest 10 % of the population rely on sales of their assets or borrowing to pay for healthcare needs (National Commission on Macroeconomics and Health, 2005 p. 3).
According to the National Healthcare Survey 2013-2014 (Global Advisory & Associated Services Pvt. Ltd, 2014) conducted amongst 12212 households and 60,000 people across twelve states;
- Insurance coverage was lowest for households with less than INR 50,000 annual income (12.23%) and highest for households earning more than INR 5, 00,000 (69.54 %)
- 81.13 % of the respondents earning annually up to INR 1,00,000 had to take loans for healthcare
Such studies and numerous others also show that hospitalization is a huge burden when it comes to annual income levels of individuals, and a single hospital stay can cost up to 40-50 percent of the per capita annual income in a public health care facility and about 80-90 % in a private health care facility (Mahal, et al., 2010). Similar fact is also highlighted in the report Health and Growth (Spence, Michael; Lewis, Maurice, 2009 p. 54) about people across the world selling productive assets and being forced into long-term poverty due to health care costs.
Cost of Hospitalization and Urban – Rural Divide in India: If we see the concentration of healthcare facilities in urban India, rural India has 68.40% of population and just 26 % (3,62,996) beds for long term care (not day care ), whereas Urban India has 31.60 % population but has 74 % (10,13,017) beds (CBHI, DGHS, MOHFW, GOI, 2012 p. 166).
The impact of the urban – rural divide on in-patient care is visible at the ground level as is evident from the following data (High Level Expert Group on Universal Health Coverage for India, 2011 p. 181).
- 11% of all episodes in rural areas and 10 % in urban areas received no healthcare at all
- 12 % of people living in rural areas and 1% in urban areas had no access to a health facility
- 28 % of rural residents and 20 % of urban residents had no funds for healthcare
- Over 40 % hospitalized persons have to borrow funds or sell assets to pay for their care
- Over 35 % of hospitalized persons fall below the poverty line because of the hospital expenses
 Geriatric Population and Hospital-based Care: The pace of growth of geriatric population is faster now (Cotlear, 2011), and India will double its proportion of people above 64 years in age over the next 25 years. Also, we need to take into account the fact that in different countries, people above the age of 65 have a higher per capita consumption on healthcare, which is between 3.4 times to 5.4 times higher than the amount spent on healthcare by people below 65 (Canada 5.4; Japan 4.9; USA 4.0; U.K. 3.4 ) (Kling, 2006). This means that the consumption of hospital based care and home care could grow manifold for India adding to the cost of healthcare, and India has not taken steps to address this issue of the impending demographic shift and its burden on the cost of healthcare delivery.
Geriatric Population and Hospital-based Care: The pace of growth of geriatric population is faster now (Cotlear, 2011), and India will double its proportion of people above 64 years in age over the next 25 years. Also, we need to take into account the fact that in different countries, people above the age of 65 have a higher per capita consumption on healthcare, which is between 3.4 times to 5.4 times higher than the amount spent on healthcare by people below 65 (Canada 5.4; Japan 4.9; USA 4.0; U.K. 3.4 ) (Kling, 2006). This means that the consumption of hospital based care and home care could grow manifold for India adding to the cost of healthcare, and India has not taken steps to address this issue of the impending demographic shift and its burden on the cost of healthcare delivery.
Private Sector and Hospitals: Private sector has 75 % of specialists and 85 % of technology in their facilities (and even as per 57 round of NSS, over 75 % of the human resources and advanced medical technology, 68 % hospitals and 37 % of the total beds are in private sector). Private sector accounts for 49 % of beds and an occupancy of 44%, whereas the public sector has occupancy of 62 % (National Commission on Macroeconomics and Health, 2005 p. 167).
Insurance coverage: About 13 % of the Indian population have some form of health insurance (Kishore, 2012 p. 34), Considering that, the Indian Government has announced two new insurance schemes; one is a cashless free scheme for accident victims (2014), and the other one is the Ayushmaan Bharat National Health Protection Mission that will provide a cover of five lakh rupees per family to about 100 million families covering a total of 500 million Indians. This scheme will subsume the two existing schemes – Rashtriya Swasthya Bima Yojana – RSBY and the Senior Citizen Health Insurance Scheme – SCHIS. (Government of India, 2018). These schemes will bring back the hospital based treatment into focus and hence, we need to be mindful of the costs associated with the hospital.
Reduction in healthcare costs by addressing the issue of hospital costs will have huge implication for the working-class families who struggle with the debt that healthcare places them under. Most working-class Indians have to fend for themselves to take care of the healthcare costs as there is no support available from the employer in terms of healthcare insurance or benefits for majority of daily-wage earners or those working for small-scale local businesses.
Hospital costs are an important aspect of this challenge and need to be addressed urgently – not only for reducing the cost of healthcare, but also for improving the quality of healthcare. Also, this is applicable for healthcare systems across the world.
Move away from the Hospital based care? Considering the fact that hospitals constitute an important chunk of the healthcare spending, should we move away from hospital based care? Not really!! In fact, the solution lies in building a healthcare system around hospital based care. Sri Lanka’s healthcare system is an interesting model.
Sri Lanka has an interesting model and an important message for the world, when it comes to how it has addressed the issue of access and healthcare for the all. It is interesting to note that Sri Lanka has better health indicators than India (World Health Organization, 2013 p. 25) and even better some European countries (Eliya, et al., 2009 p. 16), and the best health statistics in the region (High Level Expert Group on Universal Health Coverage for India, 2011 pp. 66-67), and it has expanded access to health services while reducing the government health spending as a share of GDP and it spends about 3.7 % of the GDP on healthcare (WHO, 2017) , and hospital spending accounted for 70 percent of government recurrent spending since the 1950’s.
Policy makers in Sri Lanka realized early on, that most illnesses could not be prevented and thus needed to be treated through curative interventions and thus, hospitals had toplay the lead role in combating illness and guarantee hospital care. So, they allocated budgets accordingly, so that prioritization of hospitals was an important feature of the official health policy since the 1930’s. Sri Lanka is a public hospital dominated health care system (Eliya, et al., 2009). So, in my view, the solution for lowering healthcare costs and bettering healthcare outcomes lie in managing hospital costs through publicly administered hospitals.
Lowering the cost of hospital based care is important: Given the fact, that hospital costs are a major portion of the healthcare costs, it will be important to find out what constitutes the cost centre in hospitals and which measures have led to cost reduction in hospitals.
Managing hospital costs
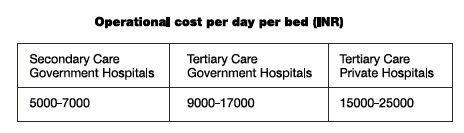
India has a shortfall of 3.5 million hospital beds (PWC, 2015), there is a dire need to study the existing models that have been successful in reducing the cost of hospitals, and it is believed that with the increase in size, the costs come down as patient outcomes are accepted to be better in hospitals where the volume of cases are more (McKee, et al., 2002 p. 100).
In India, 70 percent of Inpatient services are provided by the private hospitals but , the majority of private healthcare providers are finding it difficult to make profits in India (Gyani, 2015) The break-up of the cost of a multi-disciplinary hospital as a percentage of the net revenue is approximately as under (Gyani, 2015):
- Salary of doctors : Between 18-22 percent
- Salaries of allied health workers including nursing staff : Between 23-30 percent
- Drugs and Medical consumables : Between 28-30 percent
- Administrative cost: Between 18-20 percent
- Marketing and administrative costs : Between 5-7 percent
- Power and utilities : Between 4-5 percent
- Repair and maintenance : Between 2-3 percent
- Quality and Regulatory compliance cost : Between 2-3 percent
This implies that about 70 percent of the total operational expenditure in private hospitals is on salaries and medical consumables.
 According to the report (National Commission on Macroeconomics and Health, 2005 p. 167), an analysis of spending on health by the state Governments show that more than 70 % of the healthcare budgets are spent on salaries and wages. Another report cites that over 80 % of the recurring expenditure goes to salaries. In the case of sub-centres, often more than 80 % (some cases even more than 90 %) of the expenditure goes on account of salary for the staff (Dept of Family Welfare, GOI & The European Commission, 2004).
According to the report (National Commission on Macroeconomics and Health, 2005 p. 167), an analysis of spending on health by the state Governments show that more than 70 % of the healthcare budgets are spent on salaries and wages. Another report cites that over 80 % of the recurring expenditure goes to salaries. In the case of sub-centres, often more than 80 % (some cases even more than 90 %) of the expenditure goes on account of salary for the staff (Dept of Family Welfare, GOI & The European Commission, 2004).
It is a known fact that operational expenses represent a major cost of the healthcare projects (Taylor, 2011 p. 14).
Studies of the hospital production function have also been used to test hypotheses about economies of scale by estimating the relationship between input and output. If output increases more than an equal proportional increase in all inputs, this is obvious evidence of economies of scale”.(McKee, et al., 2002 p. 101).
Economies of scale in healthcare stands for the increased volume per given procedure being associated with enhanced outcomes which stands for higher capacity utilization and hence increased productivity (Peltokorpi, et al.).
It is observed that larger organizations may be able to bargain lower prices with their vendors and lower their cost of inputs (Given, 1996).
Economies of scale refer to a situation in which long-term average costs fall as the scale or volume of activity rises. Economies are expected to characterize a situation in which fixed costs are high relative to variable costs. As the volume of activity increases, average costs fall as fixed costs are spread over a larger base”.(McKee, et al., 2002 p. 100).
Frech and Mobley have studied and concluded that smaller hospitals could be inefficient and that larger hospitals can offer a larger bouquet and higher quality of services (Frech III, et al., 1995). Study (Marini, et al., 2009) has also brought to light the fact that by concentrating the delivery of services it can lead to cost savings, and larger hospitals can be achieving economies of scale. Also, the results favour creating larger hospital units, to facilitate intra-department, multidisciplinary working which leads to optimal use of expensive resources. Studies have supported the belief that bigger the size of the hospital better is the productivity and is economically significant. It has been analyzed that when the size of the hospital doubles, the productivity of the hospital increases by 10 % (Masayuki, 2010).
Study (Marini, et al., 2009) has also brought to light the fact that by concentrating the delivery of services it can lead to cost savings, and larger hospitals can be achieving economies of scale. Also, the results favour creating larger hospital units, to facilitate intra-department, multidisciplinary working which leads to optimal use of expensive resources. Studies have supported the belief that bigger the size of the hospital better is the productivity and is economically significant. It has been analyzed that when the size of the hospital doubles, the productivity of the hospital increases by 10 % (Masayuki, 2010).
There is growing evidence in favour of collective bargaining, volume sharing and efficiencies in care delivery leveraging purchases on behalf of a larger number of patients leading to lower costs (Lechner, et al., 2014).
There are significant to moderate long-run economies of scale for all size groups of Danish hospitals in 2004-2006. Furthermore, the ‘optimal’ number of beds per hospital is estimated to be 275 beds per site within a 95% confidence interval between 130 to 585 beds per hospital. This is roughly in line with international results”.(Kristensen, et al.).
It was studied that the larger hospitals with over 500 beds have could reduce the cost of labour in Germany (Lister, 2011 p. 20).
Insurance leads to increasing the cost of healthcare: Also, as India moves to assure health through the mega insurance scheme to cover 500 million people, it is now more important than ever before to reduce hospital costs, as the insurance experience in different parts of the world has not reduced the cost of care but lead to the increase in cost of care. Studies in China showed increased out-of-pocket expenditure for all groups in Zhenjiang (Lister, 2011 p. 73).
Efficiency can be looked at from two stand points, technical and allocation efficiency, and these can be considered either from a system or ‘macro’ perspective or from a provider or ‘micro’ perspective. Sri Lanka’s health system can be considered highly efficient, and efficiency has been an important and a critical element for its success and extending coverage (Eliya, et al., 2009 p. 16).
The OECD suggests three low-level indicators for assessing technical efficiency at the micro level : Unit costs , length of stay , and ratios of day cases to all surgery” and Sri Lanka has demonstrated that well-run government hospitals are an efficient way to deliver primary care , owing to economies of scale (Eliya, et al., 2009 p. 17).
Except for CGHS and ESIS, the other publicly funded health insurance schemes (RSBY & state insurance schemes) only cover hospitalization (Public Health Foundation of India, 2011) and it is imperative that the policy implementers in India work on this ways to reduce the cost of hospital based care.
The way forward
The study on Strategic Cost Management and Transformation in Hospitals (Kaufman, Hall & Associates, Inc.)Should be conducted in secondary and tertiary care hospitals to prepare a ‘Strategic Transformation- Best practices toolkit’.
The Strategic transformation of healthcare facilities should be done at three levels – a) Cost Management b) Administrative Process Re-engineering; and c) Clinical Transformation.
The study should focus on reviewing data for last three to five years and across specialties. The Strategic Transformation Plan should focus on;
Cost Management
Effective cost management needs a relook at the major cost heads and their relation to clinical outcomes. Also, the non-core areas may be outsourced for efficient management and removing the cost overheads attached to the hospital, as the jobs for the outsourced activities will get transferred to the contractor or vendor for the non-core services.
Administrative Process re-engineering Initiatives
Activities that focus on business restructuring offer major opportunities for cost reduction and process improvement. Which means effective business planning, manpower planning, optimum facility utilization, floor management may need re-orienting the hospital administration. Lean six-sigma could be helpful.
Clinical Transformation
Clinical transformation will need a re-calibration of processes keeping the population health, patient safety and quality of care in mind. Clinicians, support staff and the management need to work synergistically to address clinical transformation. Technology has an important role to play in effective clinical services delivery and transformation.
Since the costs for running the hospital varies according to the town class, it is imperative that the study be done across town categories, and the ‘Strategic Transformation – Best Practices Took-Kit’ be disseminated across the public facilities. This will way pave way for a major reform for hospital based healthcare in India.
Bibliography
Health Care Will Not Reform Itself [Book] / auth. Halvorson George C. – New York : Productivity Press, 2009. – p. XiX.
Sri Lanka: “Good Practice” in Expandng Health Care Coverage [Report] / auth. Eliya Ravi P. Rannan and Sikurajapathy Lankani. – Washington DC : Insitute for Health Policy, 2009. – Research Cities Series 3.
Is Quality in Healthcare , Sustainable in Developing Economies [Journal] / auth. Gyani Girdhar J // Journal of Family Medicine . – [s.l.] : Austin Publishing, December 31, 2015. – 6 : Vol. 2. – pp. 1-3.
Economies of scale and scope as an explanation of merger and output diversification activities in the health maintenance organization industry [Journal] / auth. Given S. Ruth // Journal of Health Economics. – [s.l.] : Elsevier, 1996. – pp. 685-713.
Policy Research & Analysis [Online] / auth. Lechner E, Amanda and Draper Kevin // National Institute for Health Care Reform. – 2014. – June 26, 2016. – http://www.nihcr.org/Collective-Bargaining.
New Poverty line : Rs. 32 in villages, Rs. 47 in cities [News paper] / auth. Singh Mahendra Kumar // The Times of India. – Mumbai : Bennett, Coleman & Co. Ltd., July 7, 2014. – p. 1.
The Role of Hospital management in Human Resource Development [Journal] / auth. Singh Ningombam Reagan and Debnath Arabinda // International Journal of Humanities & Social Science Studies (IJHSSS). – March 2015. – V : Vol. 1. – pp. 54-63.
Choosing Health – An entitlement for all Indians [Book] / auth. Jha Prabhat and Laxminarayan Ramanan. – Toronto : Centre for Global Health Research, 2009. – p. 14.
How Rajasthan reduced poverty [Newspaper] / auth. Mishra Mayank // Business Standard . – Bangalore : Business Standard Ltd, aUGUST 6, 2013.
The Economic Implications of Non-Communicable Diseases for India [Report] / auth. Mahal Ajay, Karan Anup and Engelgaru Michael. – Washington : HNP, The World Bank, 2010.
Is Latin America Aging [Report] / auth. Cotlear D. – Washington : The World Bank, 2011.
CRISIS OF ABUNDANCE – RETHINKING HOW WE PAY FOR HEALTH CARE [Book] / auth. Kling Arnold. – Washington : Cato Institute, 2006. – p. 21.
National Health Programs of India [Book] / auth. Kishore J. – New Delhi : Century Publications, 2012.
India [Online] / auth. Thacker Teena // The Asian Age. – June 24, 2016. – June 26, 2016. – http://www.asianage.com/india/pm-gives-nod-umbrella-health-insurance-scheme-966.
Hospitals in a Changing Europe [Report] / auth. McKee Martin and Healy Judith. – Buckingham : Open University Press , 2002. – WHO : European Observatory on Health Care Systems Series.
The Healthcare challenge [Journal] / auth. Taylor Robert // handshake. – [s.l.] : IFC, October 2011. – p. 11.
Economies of Scale and Scope in Healthcare Operations : Lessons from Surgical Services [Online] / auth. Peltokorpi Antti [et al.] // POMS Meetings. – June 26, 2016. – https://www.pomsmeetings.org/confpapers/025/025-0989.pdf.
Resolving the impasse on hospital scale economies: a new approach [Journal] / auth. Frech III H.E. and Mobley Lee Rivers // Applied Economics. – 1995. – 27. – pp. 286-296.
Economies of scale and scope in the English hospital sector – Discussion paper 2009/05 [Report] / auth. Marini Giorgia and Miraldo Marisa. – London : Imperial College Business School, 2009.
Economies of Scale and Hospital Productivity : An empirical analysis of medical area level panel data [Article] / auth. Masayuki Morikawa. – [s.l.] : The Research Institute of Economy , Trade and Industry, October 2010. – REITI Discussion Paper Series 1-E-050.
Economies of scale and optimal size of hospitals ; Empirical results for Danish public hospitals [Report] / auth. Kristensen Troels and Pedersen Moller Kjeld. – Denmark : University of Southern Denmark. – Health Economics Papers 2008:13.
Europe’s Health for Sale : The Heavy Cost of Privatisation [Book] / auth. Lister John. – Oxfordshire : Libri Publishing, 2011. – p. 3.
No health cover ? Pay 25 -60 % more [Newspaper] / auth. Thakur Pradeep // The Times of India. – Bangalore : Benett, Coleman & Co. Ltd., September 25, 2013.
McKinsey pegs poverty line at Rs.1,336 per month [Newspaper] / auth. Sinha Prabhakar // The Times of India. – New Delhi : Benett, Coleman & Co. Ltd., February 20, 2014. – p. 12.
Diabetes , heart disease treatment costs crippling poor and middle class :survey [News Paper] / auth. Nagarajan Rema // The Times of India. – Mumbai : Bennett, Coleman & Co. Ltd., October 08, 2013.
Appling Activity Based Costing (ABC) Method to Calculate Cost Price in Hospital and Remedy Services [Journal] / auth. Rajabi A and Dabiri A // Iranian Journal of Public Health. – 2012. – pp. 100-107.
Quartz India [Online] / auth. Dutta Saptarishi // The Little Chopper that could. – July 1, 2014. – July 4, 2016. – http://qz.com/228319/you-can-make-a-state-of-the-art-hospital-out-of-bamboo/%202/7.
Assam’s GNRC hospital aims big, to go global in next five years [Newspaper] / auth. Dey Supratim // Business Standard . – Guwahati : [s.n.], July 2, 2014.
High Level Expert Group Report on Universal Health Coverage for India [Report] / auth. High Level Expert Group on Universal Health Coverage for India. – New Delhi : Planning Commission of India, 2011.
National Health Expenditure Data [Online] / auth. Centers for Medicare & Medicaid Services , USA // Centers for Medicare & Medicaid Services . – December 03, 2015. – June 25, 2016. – https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/highlights.pdf.
Health Systems in Transition – Malaysia Health System Review [Report] / auth. Asia Pacific Observatory on Health Systems and Policies. – Manila : WHO -Western Pacific Region, 2012. – p. 40. – Vo. 3, No 1. 2013.
A Critical Assesment of the Existing Health Insurance Models in India [Report] / auth. Public Health Foundation of India . – New Delhi : Public Health Foundation of India , 2011. – p. 67.
National Commission on Macroeconomics and Health [Report] / auth. National Commission on Macroeconomics and Health. – New Delhi : Ministry of Health & Family Welfare, Government of India, 2005.
National Healthcare Survey 2013-2014 [Report] : Healthcare Survey / auth. Global Advisory & Associated Services Pvt. Ltd. – Mumbai : Global Advisory & Associated Services Pvt. Ltd., 2014.
Health and Growth [Report] / auth. Spence, Michael; Lewis, Maurice / Commission on Growth and Development. – Washington : World Bank, 2009.
National Health Profile 2012 [Report] : Annual / auth. CBHI, DGHS, MOHFW, GOI. – New Delhi : CBHI, DGHS, MOHFW, GOI, 2012. – p. 45.
International Business Times [Online] // News Society Politics. – August 28, 2014. – June 26, 2016. – http://www.ibtimes.co.in/government-launches-cashless-treatment-road-accident-victims-two-more-highways-607881.
World Health Statistics 2013 [Report] / auth. World Health Organization. – Geneva : WHO, 2013. – p. 14.
Future of India – The Winning Leap [Report] / auth. PWC. – New Delhi : PWC, 2015. – p. 49.
Health Sector Reforms in India [Report] / auth. Deptt of Family Welfare, GOI & The European Commission. – New Delhi : India Research Press, 2004.
Sustainable Development Goals [Online] / auth. United Nations // United Nations . – September 25, 2015. – June 25, 2016. – http://www.un.org/sustainabledevelopment/sustainable-development-goals/.
International Profiles Of Health Care Systems, 2014 [Report] / auth. The Commonwealth Fund. – Washington, DC : The Commonwealth Fund, 2015. – p. 7.
Emerging Trends in Healthcare – A Journey from Bench to Bedside [Report] / auth. KPMG ASSOCHAM. – New Delhi : KPMG, 2011. – p. 1.
Diabetes: the cost of diabetes [Online] / auth. WHO // World Health Organization. – 2013. – December 29, 2013. – http://www.who.int/mediacentre/factsheets/fs236/en/. – 236.
Healthcare I Testing Times [Newspaper] / auth. The Times of India // The Times of India. – Mumbai : Bennett, Coleman & Co. Ltd., July 13, 2014. – p. 24.
Human Development Report 2013 [Report] / auth. United Nations Development Programme. – New York : United Nations Development Programme, 2013.
National Health Profile 2011 [Report] / auth. CBHI, Ministry of Health & Family Welfare, India . – New Delhi : CBHI, Ministry of Health & Family Welfare, India , 2012.
India [Online] / auth. Oxford Poverty and Human Development Initiative (OPHI) // OPHI Country Briefing 2014 :India. – University of Oxford , June 2014. – November 26, 2014.
‘No need to set BPL for fin inclusion’ [Newspaper] / auth. TNN // The Times of India. – Mumbai : Bennett, Coleman & Co. Ltd., July 3, 2014. – p. 16.
Efficiency in Health Care: What Does it Mean ? How is it Measured ? How Can it be Used for Value-Based Purchasing? Highlights from a National Conference [Conference] / auth. AcademyHealth. – Madison : AcademyHealth, 2006. – p. 10.
Landscape of Inclusive Business Models of Healthcare in India [Report] / auth. International Finance Corporation. – New Delhi : World Bank Group, 2014.
Feature Story [Online] / auth. World Bank // The World Bank. – November 5, 2015. – July 5, 2016. – http://www.worldbank.org/en/news/feature/2015/11/05/improving-service-delivery-for-indias-poorest-waterlife-india-and-gnrc-private-hospitals.
National Portal of India [Online] / auth. Government of India // India.gov.in. – April 02, 2018. – September 09, 2018. – https://www.india.gov.in/spotlight/ayushman-bharat-national-health-protection-mission .