Remote Patient Care Beyond the Hospital: Leveraging AI and Predictive Analytics for Hospital-at-Home Programs┬Ā
The healthcare industry is experiencing a fundamental transformation as traditional hospital-centered care models evolve toward decentralized, technology-enabled approaches that bring advanced medical services directly to patients’ homes. This shift represents more than simple convenienceŌĆöit embodies a strategic response to rising healthcare costs, capacity constraints, and growing patient preferences for personalized care delivery in familiar environments. The global hospital-at-home market, valued at $8.1 billion in 2024 and projected to reach $26.8 billion by 2032, reflects the widespread recognition that remote patient care can deliver superior outcomes while reducing costs and improving patient satisfaction.┬Ā
Hospital At Home Market Data┬Ā
| Market Aspect┬Ā | Current Value┬Ā | Key Drivers┬Ā | Geographic Leaders┬Ā |
| Global Market Size 2024┬Ā | $8.1 billion┬Ā | Aging population, chronic diseases┬Ā | North America 45%┬Ā |
| Projected Market Size 2032┬Ā | $26.8 billion┬Ā | Technology advancement, cost pressure┬Ā | Asia-Pacific growth focus┬Ā |
| Market Growth Rate CAGR┬Ā | 15.20%┬Ā | Healthcare digitization┬Ā | Global expansion┬Ā |
| Patient Satisfaction Rate┬Ā | 85-92%┬Ā | Patient preference, convenience┬Ā | Developed countries┬Ā |
| Hospital Readmission Reduction┬Ā | 25-40%┬Ā | Better care coordination, monitoring┬Ā | US Medicare advantage┬Ā |
| Cost Savings vs Traditional┬Ā | 20-40%┬Ā | Reduced facility overhead┬Ā | Europe leading models┬Ā |
| Length of Stay Reduction┬Ā | 2-4 days average┬Ā | Home environment benefits┬Ā | All regions┬Ā |
| Provider Adoption Rate┬Ā | 35-45%┬Ā | Reimbursement changes┬Ā | Urban areas first┬Ā |
| Technology Investment Required┬Ā | $2-5M initial setup┬Ā | AI/IoT infrastructure needs┬Ā | Technology-advanced regions┬Ā |
| ROI Timeline┬Ā | 18-24 months┬Ā | Operational efficiency gains┬Ā | Mature healthcare systems┬Ā |
Artificial intelligence and predictive analytics serve as the technological foundation enabling this transformation, providing the monitoring capabilities, clinical decision support, and risk prediction necessary to deliver hospital-quality care in home settings.┬Ā
Remote patient care programs leverage sophisticated AI algorithms and Internet of Medical Things devices to create continuous monitoring environments that often exceed the surveillance capabilities available in traditional hospital settings. These systems can track multiple physiological parameters simultaneously, analyze patterns that might indicate developing complications, and alert healthcare providers to concerning changes before they become critical. The integration of predictive analytics enables proactive interventions that prevent hospitalizations rather than simply responding to acute episodes, fundamentally changing the care delivery paradigm from reactive to preventive medicine approaches.┬Ā
Technological Infrastructure Enabling Home-Based Care┬Ā
Comprehensive Patient Monitoring Through Connected Devices┬Ā
Modern remote patient care systems utilize an extensive array of connected devices and sensors that create comprehensive monitoring environments tailored to individual patient needs and clinical conditions. Wearable devices including smartwatches, fitness trackers, and specialized medical sensors provide continuous collection of vital signs, activity levels, sleep patterns, and medication adherence data. These devices transmit real-time information to healthcare providers through secure cloud platforms that enable immediate analysis and response to concerning trends or acute changes in patient status.┬Ā
Advanced sensor technologies extend beyond simple vital sign monitoring to encompass sophisticated environmental and behavioral tracking capabilities. Smart home sensors can monitor patient mobility patterns, detect falls or unusual activity, and assess medication compliance through intelligent pill dispensers and monitoring systems. Motion sensors and ambient monitoring devices provide insights into daily living activities, sleep quality, and behavioral changes that might indicate developing health issues or medication side effects. This comprehensive monitoring approach creates a detailed picture of patient health and functioning that often provides more complete information than periodic hospital visits or clinic appointments.┬Ā
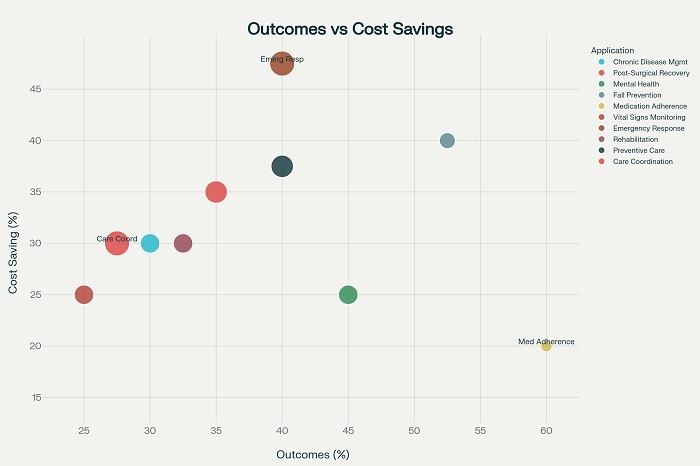
Relationship between patient outcomes improvement and cost savings across different AI-powered remote patient care applications┬Ā
The integration of artificial intelligence with these monitoring systems enables the transformation of raw data streams into clinically actionable insights. Machine learning algorithms analyze patterns across multiple data sources to identify subtle changes that might indicate disease progression, medication issues, or developing complications. These systems can establish personalized baselines for individual patients and detect deviations that warrant clinical attention, providing early warning capabilities that enable proactive interventions before serious complications develop. The predictive capabilities of these systems continue to improve as they accumulate more patient data and refine their analytical models.┬Ā
Predictive Analytics for Risk Assessment and Intervention┬Ā
Predictive analytics represents the most transformative component of modern remote patient care systems, enabling healthcare providers to identify high-risk patients and intervene before serious complications occur. Advanced algorithms analyze multiple data streams including physiological measurements, patient-reported outcomes, medication adherence patterns, and behavioral indicators to generate risk scores that predict the likelihood of hospitalization, falls, medication-related adverse events, or disease exacerbation. These predictive models enable healthcare teams to allocate resources efficiently while providing intensive monitoring and support to patients at highest risk for adverse outcomes.┬Ā
The effectiveness of predictive analytics in remote patient care has been demonstrated across multiple clinical scenarios and patient populations. Seha Virtual Hospital in Saudi Arabia utilizes predictive modeling to manage patients with chronic obstructive pulmonary disease, detecting early warning signs of exacerbations before symptoms become severe enough to require hospitalization. Similar systems have proven effective in managing heart failure patients, where subtle changes in weight, activity levels, and vital signs can predict cardiac decompensation days or weeks before traditional clinical symptoms become apparent.┬Ā
The continuous refinement of predictive models through machine learning techniques ensures that risk assessment capabilities improve over time as systems accumulate more patient data and clinical outcomes information. These self-improving systems can identify previously unrecognized patterns and risk factors while adapting to individual patient characteristics and disease progression patterns. The result is increasingly sophisticated risk stratification that enables personalized care planning and resource allocation based on individual patient needs and risk profiles.┬Ā
Clinical Applications and Disease-Specific Programs┬Ā
Chronic Disease Management and Longitudinal Care┬Ā
Chronic disease management represents the most established and successful application of AI-powered remote patient care, with programs demonstrating 25-35% reductions in hospitalizations while improving patient quality of life and treatment adherence.┬Ā
Remote Patient Care Applications┬Ā
| Application Area┬Ā | AI Technology Used┬Ā | Patient Outcomes Improvement┬Ā | Cost Savings (%)┬Ā | Implementation Complexity┬Ā |
| Chronic Disease Management┬Ā | Predictive algorithms, IoT sensors┬Ā | 25-35% reduction in hospitalizations┬Ā | 20-30%┬Ā | Medium┬Ā |
| Post-Surgical Recovery┬Ā | Wound assessment AI, activity monitoring┬Ā | 30-40% faster recovery times┬Ā | 25-35%┬Ā | Medium-High┬Ā |
| Mental Health Monitoring┬Ā | NLP sentiment analysis, behavior tracking┬Ā | 40-50% better treatment adherence┬Ā | 15-25%┬Ā | Medium┬Ā |
| Elderly Fall Prevention┬Ā | Motion sensors, predictive modeling┬Ā | 45-60% fall reduction┬Ā | 30-40%┬Ā | Low-Medium┬Ā |
| Medication Adherence┬Ā | Smart dispensers, reminder systems┬Ā | 50-70% improved compliance┬Ā | 10-20%┬Ā | Low┬Ā |
| Vital Signs Monitoring┬Ā | Wearable integration, anomaly detection┬Ā | 20-30% early intervention rate┬Ā | 15-25%┬Ā | Medium┬Ā |
| Emergency Response┬Ā | Risk scoring, automated alerts┬Ā | 35-45% faster response times┬Ā | 35-50%┬Ā | High┬Ā |
| Rehabilitation Tracking┬Ā | Movement analysis, progress tracking┬Ā | 25-40% better outcomes┬Ā | 20-30%┬Ā | Medium┬Ā |
| Preventive Care┬Ā | Health risk prediction, screening┬Ā | 30-50% early detection┬Ā | 25-40%┬Ā | Medium-High┬Ā |
| Care Coordination┬Ā | Data integration, workflow optimization┬Ā | 20-35% care efficiency gain┬Ā | 20-30%┬Ā | High┬Ā |
These programs utilize continuous monitoring to track disease-specific parameters such as blood glucose levels in diabetes, blood pressure in hypertension, and symptom patterns in chronic obstructive pulmonary disease. AI algorithms analyze these parameters in conjunction with medication adherence data, activity levels, and patient-reported symptoms to provide comprehensive disease management support that adapts to individual patient needs and preferences.┬Ā
The longitudinal nature of chronic disease management enables AI systems to develop sophisticated understanding of individual patient patterns and responses to different interventions. Machine learning algorithms can identify which medications, lifestyle modifications, and monitoring strategies prove most effective for specific patients, enabling truly personalized care plans that optimize outcomes while minimizing treatment burden. This personalized approach proves particularly valuable in managing complex patients with multiple chronic conditions where traditional one-size-fits-all approaches often prove inadequate.┬Ā
Remote patient care programs for chronic disease management also excel in providing education and self-management support that empowers patients to take active roles in their care. AI-powered chatbots and virtual assistants can provide 24/7 support for medication questions, symptom management, and lifestyle guidance while escalating complex issues to human healthcare providers when necessary. This combination of continuous monitoring and educational support creates comprehensive care environments that often exceed the capabilities available through traditional clinic-based care models.┬Ā
Post-Acute Care and Surgical Recovery┬Ā
Post-acute care represents another high-impact application area where AI-enabled remote patient care demonstrates significant advantages over traditional approaches. Surgical recovery monitoring utilizes AI-powered wound assessment tools, activity tracking systems, and pain management protocols to accelerate healing while reducing complications and readmissions. Advanced imaging algorithms can analyze wound photographs to assess healing progress, identify signs of infection, and guide treatment modifications without requiring in-person clinical visits. These systems prove particularly valuable for patients recovering from orthopedic procedures, cardiac surgery, and other complex interventions where close monitoring is essential but hospitalization is not required.┬Ā
The predictive capabilities of AI systems prove especially valuable in post-surgical settings where early identification of complications can prevent serious adverse outcomes. Machine learning algorithms can analyze patterns in vital signs, activity levels, pain scores, and wound characteristics to identify patients at risk for surgical site infections, thromboembolic complications, or other post-operative problems. Early identification enables prompt interventions that often prevent complications from progressing to severity levels requiring hospitalization or emergency department visits.┬Ā
Activity monitoring through wearable devices and smartphone applications provides objective assessment of functional recovery that often provides more accurate information than patient self-reports or periodic clinical evaluations. AI analysis of movement patterns, exercise compliance, and functional capacity changes enables healthcare providers to adjust rehabilitation protocols and identify patients who might benefit from additional physical therapy or other interventions. This objective monitoring approach ensures that patients receive appropriate support throughout their recovery process while identifying those who are progressing well enough to transition to less intensive monitoring levels.┬Ā
Implementation Strategies and Operational Considerations┬Ā
Patient Selection and Program Eligibility┬Ā
Successful implementation of AI-powered remote patient care programs requires sophisticated patient selection processes that identify individuals most likely to benefit from home-based care while ensuring safety and optimal outcomes. Machine learning algorithms can analyze multiple factors including clinical complexity, social support systems, technology proficiency, and home environment characteristics to predict successful program participation. These predictive models help healthcare providers identify patients who are appropriate candidates for remote care while ensuring that those with higher risk profiles receive more intensive monitoring or alternative care arrangements.┬Ā
The development of objective eligibility criteria reduces the labor-intensive manual chart reviews traditionally required for patient selection while improving consistency and reducing selection bias. AI-powered screening tools can rapidly analyze electronic health records, clinical data, and patient-reported information to generate eligibility scores that guide clinical decision-making. These tools prove particularly valuable in large healthcare systems where manual screening would be prohibitively time-consuming and resource-intensive.┬Ā
Geographic and logistic considerations play crucial roles in patient selection for remote care programs, with AI systems capable of incorporating factors such as distance from healthcare facilities, availability of emergency services, and local healthcare infrastructure into eligibility assessments. These comprehensive evaluation approaches ensure that remote care programs are implemented safely while maximizing their potential benefits for appropriate patient populations.┬Ā
Technology Integration and Workflow Optimization┬Ā
Effective implementation of AI-enabled remote patient care requires seamless integration with existing healthcare information systems and clinical workflows to ensure efficient data sharing and care coordination. Cloud-based platforms provide the computational power and connectivity necessary for real-time data processing while enabling scalable deployment across multiple patient populations and clinical programs. These platforms must maintain strict compliance with healthcare privacy regulations while providing healthcare providers with timely access to patient data and analytical insights.┬Ā
The integration of remote monitoring data with electronic health records ensures that all members of the healthcare team have access to comprehensive patient information that supports informed clinical decision-making. AI-powered data abstraction tools can identify the most clinically relevant information from continuous monitoring streams and present it in formats that support efficient clinical review and decision-making. This integration reduces the administrative burden on healthcare providers while ensuring that remote monitoring data enhances rather than complicates clinical workflows.┬Ā
Interoperability between different monitoring devices, software platforms, and healthcare systems represents a critical technical challenge that must be addressed to ensure program success. Standardized data formats and communication protocols enable different system components to work together effectively while providing patients with flexibility in device selection and healthcare providers with comprehensive monitoring capabilities. Investment in robust technical infrastructure and ongoing system maintenance ensures that remote care programs can adapt to evolving technology requirements and clinical needs.┬Ā
Economic Impact and Value-Based Care Alignment┬Ā
The economic benefits of AI-enabled remote patient care extend far beyond simple cost reduction to encompass fundamental improvements in care efficiency and resource utilization that align with value-based care principles. Hospital-at-home programs demonstrate cost savings of 20-40% compared to traditional inpatient care while achieving equivalent or superior clinical outcomes. These savings result from reduced facility overhead, more efficient resource utilization, and prevention of costly complications through early intervention and continuous monitoring.┬Ā
The alignment with value-based care models makes remote patient care particularly attractive to healthcare payers and providers who are increasingly focused on outcomes rather than service volume. AI-powered programs demonstrate measurable improvements in patient satisfaction, clinical outcomes, and cost efficiency that directly support value-based care objectives. The continuous monitoring and predictive capabilities of these systems enable proactive care management that prevents expensive acute care episodes while maintaining or improving patient quality of life.┬Ā
The scalability of AI-enabled remote care programs provides additional economic advantages as healthcare systems can serve larger patient populations without proportional increases in clinical staff or infrastructure investments. The technology infrastructure required for remote care programs represents a one-time investment that can support multiple clinical programs and patient populations while generating ongoing returns through improved efficiency and outcomes. This scalability makes remote care programs increasingly attractive as healthcare systems seek sustainable approaches to managing growing patient populations and clinical complexity.┬Ā
The transformation of healthcare delivery through AI-enabled remote patient care represents a fundamental shift toward personalized, proactive medicine that promises to improve outcomes while reducing costs and enhancing patient satisfaction. Success requires thoughtful implementation strategies that address technical, clinical, and operational challenges while ensuring that technology serves to enhance rather than replace human clinical expertise. As healthcare systems worldwide seek sustainable approaches to managing increasing demand and complexity, remote patient care powered by artificial intelligence and predictive analytics offers a pathway toward more efficient, effective, and patient-centered care delivery models.┬Ā



















