By Darren Jones, Country Manager, InterSystems
Electronic Medical Record (EMR) systems can enhance the efficiency and performance of healthcare services by streamlining care workflows, promoting interdisciplinary working, and providing on-demand access to comprehensive patient information across healthcare teams.
EMR systems also provide a platform for more connected and patient-centric models of care across large geographies or populations, even though their impact in supporting this sort of care delivery reform has been limited to date.
Reported benefits of EMR solutions include improved patient safety, clinical outcomes, service efficiency, financial performance, and patient experience. These typically derive from improvements in care documentation, medication management, service insights and compliance, capacity and demand management, and patient communication, as well as reduced incidence of delayed or inappropriate care decisions.
However, achieving these benefits requires high levels of adoption by frontline staff and an ongoing program of value measurement and solution optimisation. Further, to realise value from technological advances like Artificial Intelligence (AI) and new service delivery models, EMR solutions must be architected with evolution and change in mind.
Realising value from EMR systems
While much evidence supports the value of EMR systems, their implementation can be challenging, requiring well-executed change management involving meaningful and continued engagement with time-poor staff.
EMR deployments often focus on organisational value, typically detailed by a business case. Frontline staff often have to extrapolate meaning for their day-to-day working practices, which may or may not happen. Staff can be challenged by change without understanding its value to them as individuals, resulting in poor motivation and change management difficulties.
Articulating value in terms that resonate with frontline staff can help maintain momentum and enthusiasm for change. Established techniques from other industries, such as persona analysis, provide a helpful tool to express role-specific value definitions.
Collecting qualitative and quantitative data is also fundamental in evidencing and communicating the value of a EMR solution. It is good practice to plan and action this activity before going live. This establishes credible baseline data to compare against post go-live data to determine the value delivered and any unanticipated negative value for prioritisation in continuous improvement programs.
An ongoing journey, not an event
The delivery and articulation of value is not an event but an ongoing journey. Post go-live analysis may focus upon a defined set of benefit and outcome measures, possibly described by the original business case. But an ongoing program of solution optimisation and value measurement helps to ensure the solution evolves with service needs, whilst identifying underperforming aspects that require corrective intervention.
An important post go-live dataset, commonly overlooked, relates to solution adoption and activity. This highlights areas of functionality and configuration that perform well or those requiring further interventions like user training or solution configuration changes. Automated adoption dashboards (see Figure 1) also provide dynamic insights.
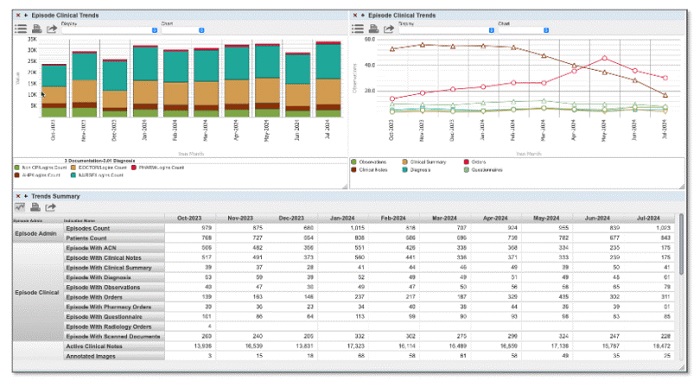
Figure 1 – Example post go-live adoption dashboard
EMRs must evolve to support new value
All EMR solutions will continue to be shaped by technological innovation and changing healthcare demands. A solution’s long-term success will depend on quickly and cost-effectively supporting new value opportunities presented by advances in technology, science, and service delivery models.
AI and Machine Learning (ML), for example, present realistic and affordable options to enhance the quality and outcomes of care interventions. In fact, it is hard to imagine an enterprise-scale EMR solution without AI capabilities in two years’ time.
Generative AI solutions already help care professionals consolidate, synthesise, and summarise patient record data to improve the efficiency and precision of care planning and interventions. ML examples include predictive analysis, such as identifying patients at a higher risk of readmission, developing conditions, or unexpected deterioration.
Integrating interoperability standards, such as Fast Healthcare Interoperability Resources (FHIR), will also become crucial. These facilitate the sharing of structured, coded, and actionable patient information across health and social care services. This is particularly important in enhancing the efficiency and effectiveness of care transitions and collaborative decision-making across large geographies or populations.
Enterprise EMR solutions will also evolve to provide genomic capabilities relating to test orders and results and, importantly, pharmacogenomic decision support to guide and inform the correct and appropriate use of medications for each individual. This understanding, combined with EMR technology, has the potential to transform care outcomes on a scale similar to the introduction of antibiotics.
Transformation and new models of care
The term ‘digital transformation’ is hard to escape. But what does this mean for healthcare services adopting an EMR solution?
Digital transformation represents an organisational re-wiring to create value for the organisation and its consumers via innovative business models. However, while many initiatives deliver modernised healthcare interventions – such as video consultations, virtual wards, healthcare apps, and AI technologies – these have been primarily used to enhance existing models of care.
Recognition of the need for new models of care that reflect the demands of modern societies is rapidly gaining pace. Current integrated care models rely on the ability of EMR platform technologies to support the seamless flow of information across healthcare services for the planning, management, allocation, and delivery of healthcare interventions (see Figure 2).
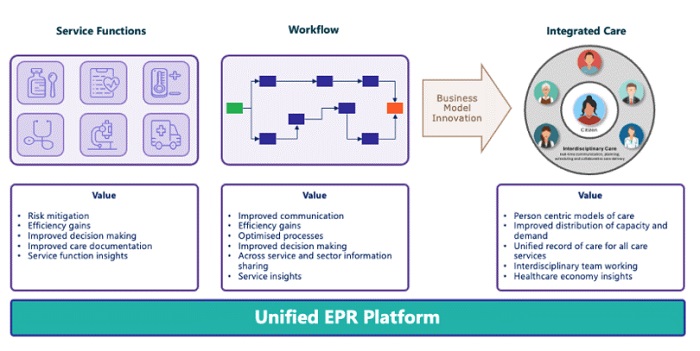
Figure 2 – EMR-enabled integrated care model transformation
The transformation of healthcare to deliver genuinely patient-centric and joined-up care workflows will require significant service reforms and a paradigm shift. In particular, it will require moving away from the dominance of acute care. Working in interdisciplinary teams spanning care sectors will also be a significant change and challenge for healthcare professionals.
EMR solutions must provide a critical enabling and supportive role for the unimpeded flow of information across a healthcare region to inform the joined-up planning, management, allocation, and delivery of timely and appropriate care interventions.
Whilst the value currently delivered by EMR solutions is significant and important, the overwhelming value for a modern-day EMR system is in supporting the new and emerging models of care we so desperately need.
About the author
Darren Jones is Country Manager, Australia and New Zealand at InterSystems, a creative data technology provider which delivers a unified foundation for next-generation applications for healthcare, finance, manufacturing and supply chain customers in more than 80 countries, and electronic medical record systems which support advanced data management in hospitals. Based in Melbourne, Jones leads the company’s operations in Australia and New Zealand and supports the success of InterSystems customers.




















