The transformation of hospitals into fully connected healthcare ecosystems represents one of the most significant operational shifts in modern medicine, fundamentally changing how medical devices interact, share information, and support patient care delivery. As healthcare organizations increasingly deploy Internet of Things medical devices across their facilities, from smart infusion pumps to wireless patient monitors, the challenge extends far beyond simply connecting devices to networks. Success in creating truly connected hospital IoT medical devices requires sophisticated integration strategies that address interoperability, security, workflow optimization, and data management while maintaining the highest standards of patient safety and care quality.
The scale of this transformation is unprecedented in healthcare history. Modern hospitals may manage thousands of connected devices across multiple departments, each generating continuous streams of data that must be collected, processed, and integrated into clinical workflows. The complexity multiplies when considering that these devices often come from different manufacturers, operate on various communication protocols, and must interface with existing hospital information systems that were never designed for such extensive connectivity.
Hospital administrators face the daunting task of orchestrating these complex integrations while ensuring that connectivity enhances rather than complicates clinical care. The stakes are particularly high because poorly managed device integration can create workflow bottlenecks, generate alert fatigue among staff, compromise patient safety, or expose sensitive health information to cybersecurity threats. Understanding and mastering the principles of effective IoT medical device integration has become essential for hospital leaders seeking to realize the benefits of connected healthcare while avoiding potential pitfalls.
Understanding the Connected Hospital Ecosystem
The modern connected hospital encompasses a vast network of intelligent medical devices that communicate with each other, hospital information systems, and cloud-based platforms to create an integrated healthcare environment. This ecosystem extends beyond traditional medical equipment to include environmental sensors, asset tracking systems, workflow optimization tools, and patient engagement platforms that work together to support comprehensive care delivery.
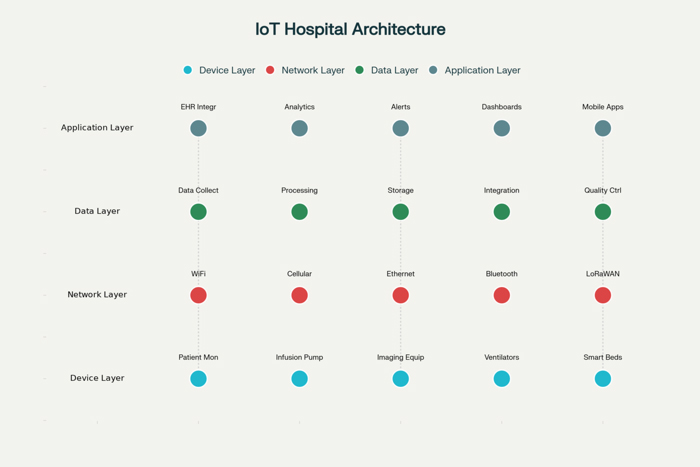
Connected hospital IoT medical devices operate within multiple layers of infrastructure that must work seamlessly together to ensure effective integration. The physical layer includes the devices themselves, along with networking hardware, wireless access points, and communication protocols that enable device connectivity. The data layer encompasses the systems and processes that collect, store, and manage the enormous volumes of information generated by connected devices, while the application layer includes the software systems that analyze device data and present actionable insights to healthcare professionals.
Interoperability challenges emerge as one of the most complex aspects of connected hospital management because medical devices traditionally operated as standalone systems with limited communication capabilities. Modern integration efforts must bridge significant gaps between legacy equipment and newer connected devices while ensuring that different manufacturer systems can exchange information effectively. This interoperability extends beyond technical communication to encompass semantic interoperability, where systems must not only share data but understand the meaning and context of that information.
The clinical workflow integration dimension adds another layer of complexity because connected devices must support rather than disrupt established care processes. Healthcare professionals have developed sophisticated routines and protocols over years of practice, and successful device integration must respect these workflows while providing new capabilities that enhance rather than complicate clinical decision-making. This requires deep understanding of how different medical specialties operate and how connected devices can be configured to align with existing practices.
Device Discovery and Inventory Management
Effective management of connected hospital IoT medical devices begins with comprehensive discovery and inventory processes that provide complete visibility into all connected assets within the healthcare environment. This visibility serves as the foundation for security, compliance, and operational management because administrators cannot protect or optimize devices they cannot identify and track systematically.
Modern hospital environments present unique challenges for device discovery because medical IoT devices may connect through various network pathways, including wireless networks, cellular connections, Bluetooth protocols, and direct ethernet connections. Each connection type requires different discovery approaches and monitoring strategies to ensure complete asset visibility. Additionally, many medical devices operate intermittently or move between locations, complicating traditional network scanning approaches.
Automated discovery systems have become essential for managing the scale and complexity of connected hospital environments because manual inventory processes cannot keep pace with the dynamic nature of modern medical device deployments. These systems must be capable of identifying not only the presence of connected devices but also their specific configurations, software versions, security status, and operational parameters. This detailed information enables administrators to make informed decisions about device management, security policies, and integration strategies.
The classification and categorization of discovered devices requires sophisticated understanding of medical device types, clinical applications, and risk profiles because different devices require different management approaches. Critical life-support equipment demands higher security and monitoring standards than environmental sensors, while patient-facing devices may require different privacy protections than administrative systems. Effective inventory management systems must capture these distinctions and enable policy application based on device categories and risk levels.
Security Architecture for Connected Medical Devices
The security architecture for connected hospital IoT medical devices must address unique challenges that distinguish healthcare environments from other industries while providing robust protection against increasingly sophisticated cyber threats. Medical device security extends beyond traditional information technology concerns to encompass patient safety considerations because compromised devices can directly impact clinical care and potentially endanger patient lives.
Network segmentation emerges as a fundamental security strategy for connected hospital environments because it provides isolation between different types of devices and systems while enabling necessary communication pathways. Medical IoT devices should operate on dedicated network segments that separate them from general hospital computing systems and external internet access while providing controlled pathways for essential integrations with Electronic Health Records and clinical applications.
Authentication and authorization frameworks for medical devices require careful balance between security requirements and operational realities because healthcare environments demand rapid access during emergency situations while maintaining strict controls over device access and configuration. Multi-factor authentication, certificate-based device identity, and role-based access controls must be implemented in ways that support rather than impede clinical workflows while ensuring that only authorized personnel can access or modify device settings.
Encryption protocols for medical device communications must protect sensitive patient data during transmission while accommodating the performance limitations of many medical IoT devices that have constrained processing capabilities. End-to-end encryption, secure key management, and regular credential rotation become essential components of comprehensive security strategies, but implementation must consider the operational impact on device performance and battery life.
The vulnerability management process for connected medical devices presents unique challenges because traditional software patching approaches may not be appropriate for life-critical medical equipment that requires extensive testing and validation before updates can be applied. Healthcare organizations must develop sophisticated vulnerability assessment processes that prioritize risks based on device criticality, patient impact, and available mitigation strategies while coordinating with device manufacturers and regulatory authorities.
Interoperability Standards and Protocols
Achieving effective interoperability among connected hospital IoT medical devices requires adherence to established healthcare standards and protocols that enable seamless data exchange while preserving the semantic meaning of clinical information. The complexity of healthcare interoperability extends beyond technical communication to encompass the medical terminology, data structures, and workflow patterns that define how healthcare information should be organized and interpreted.
Health Level Seven International standards, particularly HL7 FHIR, have emerged as critical enablers of medical device interoperability because they provide standardized approaches for representing and exchanging healthcare information in ways that preserve clinical context and meaning. These standards enable connected devices to communicate with Electronic Health Record systems, clinical decision support applications, and other healthcare technologies while maintaining data integrity and clinical relevance.
The Digital Imaging and Communications in Medicine standard continues to play essential roles in connecting medical imaging devices and systems, but modern implementations must accommodate IoT integration requirements including cloud connectivity, mobile access, and real-time streaming capabilities. DICOM integration with IoT platforms enables connected imaging devices to automatically route studies, trigger workflow events, and integrate with artificial intelligence analysis tools.
IEEE 11073 standards specifically address personal health devices and point-of-care medical equipment interoperability, providing frameworks for connecting devices like patient monitors, infusion pumps, and wearable sensors to hospital information systems. These standards define communication protocols, data formats, and device profiles that enable plug-and-play connectivity while ensuring clinical data quality and patient safety.
Emerging interoperability frameworks must address the growing complexity of connected hospital environments where devices from multiple manufacturers must work together seamlessly while accommodating different connectivity options, data formats, and security requirements. Modern interoperability solutions increasingly rely on API-driven architectures, cloud-based integration platforms, and edge computing capabilities that can manage the real-time demands of connected medical devices.
Data Management and Analytics Integration
The management of data generated by connected hospital IoT medical devices requires sophisticated approaches that can handle the volume, velocity, and variety of information flowing from numerous connected sources while extracting actionable insights that support clinical decision-making and operational optimization. Modern connected hospitals may generate terabytes of device data daily, creating both opportunities and challenges for healthcare organizations seeking to leverage this information effectively.
Real-time data processing capabilities become essential for connected hospital environments because many medical IoT devices generate time-sensitive information that requires immediate analysis and response. Patient monitoring devices, for example, must be able to trigger immediate alerts when vital signs exceed safe parameters, while infusion pumps need real-time integration with medication management systems to ensure accurate dosing and prevent adverse drug events.
Data integration platforms must be capable of normalizing and correlating information from diverse connected devices while maintaining the clinical context and quality necessary for healthcare decision-making. This integration extends beyond simple data aggregation to include sophisticated processing that can identify patterns, detect anomalies, and generate insights that would be impossible from isolated device data streams.
The storage and retention of IoT medical device data must comply with healthcare regulations while providing the accessibility and performance required for clinical and operational applications. Cloud-based storage solutions offer scalability advantages but must address data sovereignty, privacy, and security requirements that govern healthcare information management. Hybrid approaches that combine on-premises and cloud storage can provide flexibility while maintaining compliance with regulatory requirements.
Analytics applications for connected hospital IoT medical devices must provide actionable insights that support both clinical care and operational management while avoiding information overload that can overwhelm healthcare professionals. Successful analytics implementations focus on delivering the right information to the right people at the right time through intuitive interfaces that integrate with existing clinical workflows and decision-making processes.
Workflow Integration and User Experience
The integration of connected hospital IoT medical devices into clinical workflows represents one of the most critical success factors for healthcare technology implementations because devices that disrupt established care processes often face resistance and underutilization regardless of their technical capabilities. Effective workflow integration requires deep understanding of how healthcare professionals operate and how connected devices can enhance rather than complicate existing care delivery patterns.
Clinical workflow analysis must precede device integration planning because successful implementations build upon rather than replace established care processes that have evolved to ensure patient safety and operational efficiency. This analysis should identify decision points, information needs, and communication patterns that connected devices can support while recognizing workflow variations across different clinical specialties and care settings.
User interface design for connected medical devices becomes increasingly important as healthcare professionals interact with growing numbers of connected systems throughout their daily routines. Consistent interface paradigms, intuitive navigation patterns, and role-based information presentation help reduce the cognitive burden associated with managing multiple connected devices while ensuring that critical information remains accessible during high-stress clinical situations.
Alert management strategies must balance the need for timely notification of important events with the growing problem of alert fatigue that can reduce healthcare professional responsiveness to critical warnings. Connected hospital IoT medical devices can generate overwhelming numbers of alerts if not properly configured and prioritized, requiring sophisticated alert correlation, escalation, and suppression capabilities that ensure important information reaches the right people without creating noise.
Mobile integration capabilities become essential for connected hospital environments because healthcare professionals are highly mobile and need access to device information and controls regardless of their physical location within the facility. Mobile applications and responsive web interfaces must provide secure, real-time access to connected device data while accommodating the diverse device preferences and workflow patterns of different healthcare roles.
Regulatory Compliance and Quality Assurance
The regulatory landscape for connected hospital IoT medical devices encompasses complex requirements from multiple authorities including the Food and Drug Administration, the Federal Communications Commission, and healthcare privacy regulators that must be navigated carefully to ensure compliant implementations. These regulatory requirements often interact in complex ways that require comprehensive compliance strategies addressing device approval, network operation, and data protection simultaneously.
FDA oversight of connected medical devices continues evolving as the agency develops frameworks for regulating software-driven medical technologies and cybersecurity requirements for connected devices. Healthcare organizations must understand how device connectivity affects regulatory classification and compliance obligations while working with manufacturers to ensure that integration approaches maintain device approvals and safety certifications.
HIPAA compliance for connected medical devices requires careful attention to how patient health information is collected, transmitted, stored, and accessed through IoT systems because traditional privacy protections may not adequately address the unique characteristics of connected device environments. Business associate agreements, access controls, audit logging, and breach notification procedures must be adapted for connected device contexts while maintaining the privacy protections that patients expect and regulations require.
Quality assurance processes for connected hospital IoT medical devices must address both the technical performance of individual devices and the integrated performance of connected systems that work together to support patient care. Traditional device testing approaches may not adequately evaluate how devices perform within connected environments where network conditions, integration points, and workflow patterns can significantly impact device behavior and clinical outcomes.
Risk management frameworks must evolve to address the unique risk profiles associated with connected medical devices including cybersecurity threats, interoperability failures, data quality issues, and cascade failures where problems with one connected device can impact other systems. These frameworks should provide systematic approaches for identifying, assessing, and mitigating risks while maintaining the benefits that connectivity provides for patient care and operational efficiency.
Performance Monitoring and Optimization
Effective management of connected hospital IoT medical devices requires continuous monitoring and optimization processes that ensure devices operate at peak performance while identifying opportunities for improvement in clinical outcomes and operational efficiency. Performance monitoring extends beyond traditional uptime metrics to encompass clinical effectiveness, user satisfaction, and integration quality measures that reflect the comprehensive impact of connected devices on healthcare delivery.
Network performance monitoring becomes critical for connected hospital environments because device connectivity depends on reliable, high-performance network infrastructure that can support the real-time demands of medical IoT applications. Bandwidth utilization, latency measurements, and connectivity reliability metrics must be tracked continuously to identify potential problems before they impact clinical care or device functionality.
Device health monitoring systems must track the operational status of individual connected devices while correlating performance data across integrated systems to identify patterns and trends that might indicate emerging problems. Predictive maintenance capabilities can help healthcare organizations address device issues proactively rather than reactively, reducing downtime and improving reliability for patient care applications.
Clinical outcome measurements should evaluate how connected hospital IoT medical devices contribute to improved patient care, reduced medical errors, enhanced efficiency, and better healthcare professional satisfaction. These measurements provide essential feedback for optimization efforts while demonstrating the value proposition for connected device investments to hospital administrators and clinical stakeholders.
Optimization strategies for connected medical devices must balance multiple competing objectives including clinical effectiveness, user satisfaction, operational efficiency, security requirements, and cost considerations. Successful optimization requires iterative approaches that involve healthcare professionals in identifying improvement opportunities while leveraging data analytics to guide enhancement priorities and measure results.
The future of connected hospital IoT medical devices lies in creating truly intelligent healthcare environments where connected systems work together seamlessly to support patient care while reducing administrative burden and improving operational efficiency. Organizations that master the complex integration challenges associated with connected medical devices position themselves to deliver superior patient outcomes while building foundations for continued innovation and improvement in healthcare delivery.



















