Scaling Remote Patient Monitoring: From Pilot to System-Wide Implementation
The journey from successful remote patient monitoring pilot programs to comprehensive system-wide implementation represents one of the most challenging yet critical transitions in modern healthcare technology adoption. While many healthcare organizations excel at launching focused remote monitoring initiatives that demonstrate impressive results within limited populations, scaling remote patient monitoring systems across entire health networks requires fundamentally different strategies, resources, and organizational capabilities. The complexity of this transformation extends far beyond simply adding more devices or enrolling additional patients, demanding sophisticated approaches to workflow integration, technology infrastructure, clinical governance, and change management that can sustain growth while maintaining quality and safety standards.
The urgency surrounding remote patient monitoring expansion has intensified as healthcare organizations face mounting pressures from aging populations, increasing chronic disease prevalence, and evolving value-based care models that reward improved outcomes and cost efficiency. Current statistics indicate that over 71 million Americans are expected to utilize remote patient monitoring services by 2025, with the global market projected to reach $115.5 million users by 2027. These projections underscore the reality that healthcare organizations must move beyond experimental approaches to develop scalable, sustainable remote monitoring programs that can accommodate rapid growth while delivering consistent clinical value.
Hospital administrators and healthcare executives increasingly recognize that successful scaling remote patient monitoring systems requires comprehensive strategic planning that addresses technology infrastructure, clinical workflow integration, staff training, regulatory compliance, and financial sustainability simultaneously. Organizations that approach scaling initiatives with appropriate planning and resources consistently achieve better outcomes than those attempting to expand programs through organic growth or ad hoc approaches. Understanding the principles and practices that enable successful remote monitoring expansion has become essential for healthcare leaders seeking to realize the full potential of these transformative technologies.
Strategic Planning for Remote Monitoring Expansion
The foundation of successful scaling remote patient monitoring systems lies in comprehensive strategic planning that establishes clear objectives, identifies target populations, defines success metrics, and creates roadmaps for sustainable growth. This planning process must balance ambitious expansion goals with realistic assessments of organizational capabilities, resource constraints, and market conditions that influence the feasibility and timeline of scaling initiatives.
Market analysis becomes essential for organizations seeking to understand the demand for remote monitoring services within their patient populations while identifying opportunities for expansion across different clinical specialties and patient demographics. This analysis should examine chronic disease prevalence, readmission patterns, patient satisfaction scores, and competitor activities that might influence the success of remote monitoring programs while providing data-driven insights for expansion planning.
Stakeholder engagement throughout the planning process ensures that scaling initiatives address the needs and concerns of diverse constituents including physicians, nurses, administrators, patients, and technology partners who will contribute to program success. Early involvement of these stakeholders in planning discussions helps identify potential obstacles, resource requirements, and implementation strategies that support rather than complicate existing workflows and clinical practices.
The development of comprehensive business cases for remote monitoring expansion must demonstrate both clinical value and financial sustainability while addressing implementation costs, operational expenses, revenue opportunities, and return on investment projections. These business cases should include detailed analysis of reimbursement opportunities, cost savings potential, competitive advantages, and strategic alignment with organizational objectives that justify the investments required for successful scaling.
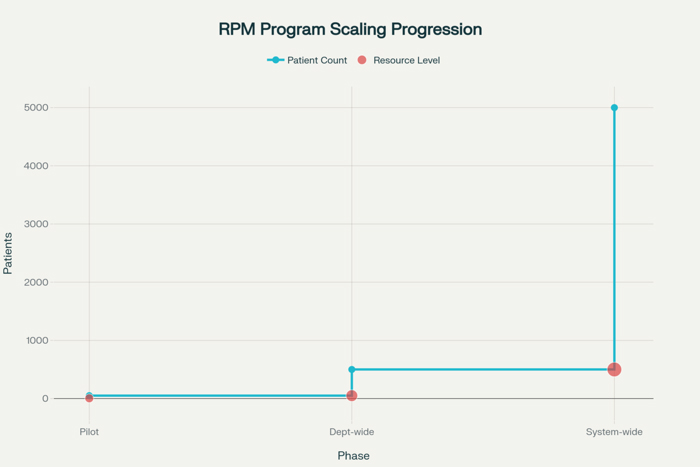
Resource allocation planning for scaling remote patient monitoring systems must address technology infrastructure, staffing requirements, training programs, and ongoing operational support needed to sustain expanded programs. This planning should consider both immediate scaling needs and future growth projections to ensure that infrastructure investments can accommodate continued expansion without requiring frequent major upgrades or replacements.
Technology Infrastructure and Platform Selection
Scalable technology infrastructure represents the backbone of successful remote patient monitoring expansion because inadequate platforms or systems cannot accommodate the growth demands associated with system-wide implementation. Organizations must evaluate their current technology capabilities and identify gaps that could limit scaling success while developing comprehensive technology strategies that support both immediate expansion needs and long-term growth objectives.
Platform scalability assessment requires detailed evaluation of current remote monitoring systems to determine their capacity for handling increased patient volumes, expanded device types, additional clinical specialties, and enhanced analytical capabilities that support larger programs. This assessment should examine system architecture, database capabilities, integration options, and performance characteristics under various load conditions to identify potential bottlenecks or limitations that could impede scaling success.
Integration capabilities become increasingly important as remote monitoring programs expand across multiple departments and clinical specialties that may utilize different Electronic Health Record systems, clinical applications, and workflow processes. Successful scaling requires seamless integration between remote monitoring platforms and existing hospital information systems to ensure that expanded programs enhance rather than complicate clinical workflows and decision-making processes.
Data management strategies for scaled remote monitoring programs must address the exponential growth in data volume, velocity, and variety that accompanies program expansion while ensuring that clinical teams receive actionable insights without experiencing information overload. These strategies should include automated data processing, intelligent alerting systems, and analytical dashboards that enable effective monitoring of large patient populations while maintaining personalized care capabilities.
Cloud computing considerations become particularly relevant for scaling remote patient monitoring systems because cloud platforms can provide the flexibility, scalability, and cost-effectiveness necessary for supporting rapid program growth. Organizations must evaluate cloud options carefully to ensure they meet healthcare-specific requirements for security, compliance, performance, and integration while providing the scalability advantages necessary for successful expansion.
Clinical Workflow Integration and Standardization
The successful scaling of remote patient monitoring systems demands comprehensive integration with existing clinical workflows while establishing standardized processes that ensure consistent care quality across expanded programs and diverse clinical settings. This integration challenge requires careful analysis of current workflows, identification of optimization opportunities, and development of standardized procedures that support rather than disrupt established clinical practices.
Workflow standardization across multiple departments and clinical specialties becomes essential for scaling remote patient monitoring systems because inconsistent processes can create confusion, reduce efficiency, and compromise care quality as programs expand. Standardized workflows should address patient enrollment, device deployment, data monitoring, clinical response protocols, and care coordination while allowing for appropriate customization based on specialty-specific requirements.
Clinical decision support integration enables healthcare providers to leverage remote monitoring data effectively within their existing decision-making processes while providing the analytical capabilities necessary for managing larger patient populations. These systems should provide intelligent alerting, trend analysis, risk stratification, and care recommendations that enhance clinical judgment without creating alert fatigue or workflow disruptions.
The development of clinical protocols for scaled remote monitoring programs must address various patient populations, clinical conditions, and care scenarios while ensuring that all providers have clear guidance for utilizing remote monitoring data in clinical decision-making. These protocols should establish standards for data interpretation, response timeframes, escalation procedures, and care coordination that maintain clinical quality as programs expand.
Training and competency development programs become increasingly important as remote monitoring programs scale because larger programs typically involve more healthcare providers with varying levels of technology comfort and remote monitoring experience. These programs should address both technical proficiency and clinical application skills while providing ongoing education that keeps pace with program evolution and technology advancement.
Patient Engagement and Population Management
Effective patient engagement strategies become increasingly complex but critically important as remote monitoring programs scale because larger patient populations bring greater diversity in demographics, health literacy levels, technology comfort, and engagement preferences. Successful scaling requires sophisticated approaches to patient recruitment, onboarding, education, and ongoing engagement that can accommodate this diversity while maintaining high participation and adherence rates.
Population health management capabilities enable healthcare organizations to leverage remote monitoring data for identifying trends, predicting risks, and implementing preventive interventions across large patient populations. These capabilities should include predictive analytics, risk stratification algorithms, and population health dashboards that enable proactive care management while supporting value-based care initiatives and quality improvement programs.
Patient segmentation strategies help organizations tailor remote monitoring approaches to different patient groups based on clinical conditions, risk levels, technology preferences, and engagement capabilities. Effective segmentation enables more personalized care delivery while optimizing resource allocation and ensuring that high-risk patients receive appropriate levels of monitoring and intervention.
Multilingual and culturally appropriate engagement approaches become essential as remote monitoring programs expand to serve diverse patient populations with varying linguistic, cultural, and socioeconomic characteristics. These approaches should address language barriers, cultural preferences, and accessibility considerations that could impact program participation and effectiveness among different patient groups.
Automated engagement systems help healthcare organizations maintain consistent patient communication and support across large remote monitoring populations while reducing the manual workload associated with program management. These systems should include automated reminders, educational content delivery, adherence monitoring, and escalation protocols that ensure patients receive appropriate support throughout their remote monitoring experience.
Quality Assurance and Clinical Governance
Maintaining clinical quality and safety standards becomes increasingly challenging as remote monitoring programs scale because larger programs create more opportunities for errors, inconsistencies, and adverse events while requiring more sophisticated oversight and governance mechanisms. Organizations must develop comprehensive quality assurance frameworks that ensure expanded programs maintain the clinical excellence and patient safety standards established during pilot phases.
Clinical governance structures for scaled remote monitoring programs must establish clear accountability, oversight mechanisms, and decision-making processes that ensure appropriate clinical leadership and quality management across expanded programs. These structures should include clinical advisory committees, quality improvement teams, and safety oversight groups that provide ongoing guidance and oversight for program operations.
Performance monitoring systems enable healthcare organizations to track clinical outcomes, safety metrics, operational efficiency, and patient satisfaction across scaled remote monitoring programs while identifying trends and opportunities for improvement. These systems should provide real-time dashboards, automated reporting capabilities, and analytical tools that support data-driven quality improvement initiatives.
Risk management frameworks for scaled remote monitoring programs must address the unique risks associated with remote care delivery while providing systematic approaches for identifying, assessing, and mitigating potential safety concerns. These frameworks should include incident reporting systems, risk assessment protocols, and corrective action procedures that ensure patient safety throughout expanded programs.
Regulatory compliance management becomes more complex as remote monitoring programs scale because larger programs may span multiple jurisdictions, serve diverse patient populations, and utilize various technologies that must comply with different regulatory requirements. Organizations must develop comprehensive compliance programs that address HIPAA requirements, FDA regulations, state licensing requirements, and other applicable standards while maintaining operational efficiency.
Financial Management and Sustainability
The financial sustainability of scaled remote monitoring programs requires sophisticated approaches to cost management, revenue optimization, and return on investment analysis that address the complex economics of expanded programs while ensuring long-term viability. Organizations must develop comprehensive financial strategies that balance growth investments with operational efficiency while maximizing reimbursement opportunities and demonstrating value to stakeholders.
Cost structure analysis for scaled remote monitoring programs must address both fixed and variable costs associated with technology infrastructure, staffing, training, devices, and ongoing operations while identifying opportunities for economies of scale and operational efficiencies. This analysis should provide detailed understanding of cost drivers and optimization opportunities that support sustainable growth while maintaining clinical quality.
Revenue optimization strategies enable healthcare organizations to maximize reimbursement opportunities associated with remote monitoring services while exploring innovative payment models that support program sustainability. These strategies should address Medicare and Medicaid reimbursement codes, commercial payer negotiations, value-based care contracts, and shared savings opportunities that provide financial incentives for remote monitoring programs.
Return on investment calculations for scaled remote monitoring programs must demonstrate financial value while accounting for both direct cost savings and indirect benefits such as improved patient outcomes, reduced readmissions, enhanced patient satisfaction, and competitive advantages. These calculations should provide compelling evidence for continued investment in program expansion while identifying factors that contribute to financial performance.
Budget planning and resource allocation for scaling initiatives requires careful balance between growth investments and operational sustainability while ensuring that financial resources are allocated effectively to support program objectives. This planning should address both short-term scaling needs and long-term sustainability requirements while providing flexibility for adapting to changing conditions and opportunities.
Performance Measurement and Optimization
Comprehensive performance measurement systems enable healthcare organizations to track the success of scaling remote patient monitoring systems while identifying opportunities for optimization and continuous improvement. These measurement systems must address clinical outcomes, operational efficiency, patient satisfaction, and financial performance while providing actionable insights that guide program development and resource allocation decisions.
Key performance indicators for scaled remote monitoring programs should encompass clinical effectiveness metrics such as readmission rates, emergency department utilization, medication adherence, and patient outcomes while including operational measures such as program enrollment, device utilization, alert response times, and staff productivity. These indicators provide comprehensive assessment of program performance while identifying areas requiring attention or improvement.
Benchmarking and comparative analysis enable organizations to assess their remote monitoring program performance against industry standards, best practices, and peer organizations while identifying opportunities for improvement and optimization. This analysis should include both clinical and operational benchmarks that provide context for performance evaluation and guide improvement initiatives.
Continuous improvement processes for scaled remote monitoring programs must incorporate regular performance review cycles, stakeholder feedback, and data-driven optimization initiatives that ensure programs evolve and improve over time. These processes should include systematic approaches for identifying improvement opportunities, implementing changes, and measuring results while maintaining focus on clinical quality and patient safety.
Data analytics capabilities enable healthcare organizations to extract insights from the vast amounts of data generated by scaled remote monitoring programs while identifying trends, patterns, and opportunities that support evidence-based decision-making. These capabilities should include predictive analytics, population health analysis, and operational intelligence that enhance program effectiveness while supporting strategic planning and quality improvement initiatives.
The path forward for scaling remote patient monitoring systems requires sustained commitment to comprehensive program development that addresses technology infrastructure, clinical integration, patient engagement, quality assurance, financial sustainability, and performance optimization while maintaining focus on improved patient outcomes and care quality. Organizations that successfully navigate these scaling challenges position themselves to deliver superior healthcare services while achieving operational excellence and financial sustainability in an increasingly competitive and value-focused healthcare environment.


















