Sedation is one of the most imperative skills to acquire to ensure patient safety and comfort. However, lack of formal training remains an issue. That is why safe sedation training is an important part of medical education. Such training typically involves a professional course focusing on the skills and competencies of safe sedation practice, which guides clinicians in managing patients before, during, and after sedation administration.
Sedation training programs in various sectors of medical disciplines have been implemented with guidelines to ensure the highest level of patient care. Modern sedation training passes on knowledge of best moderate sedation clinical practices and, with innovation, uses human simulators and accelerated learning.
Sedation in Various Medical Roles
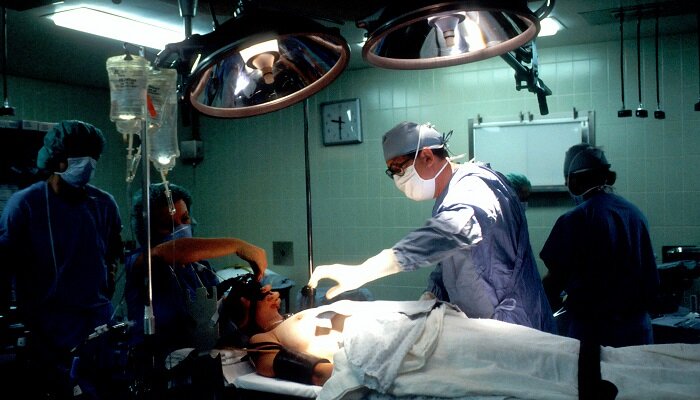
From dentistry to physician assistants, medical professionals use sedation in varying ways. Together, these roles offer distinct advantages for providing safe and effective sedation. They allow training adapted to the specific requirements of each medical discipline and enable healthcare providers to take a more active and direct role in sedation management that better supports patient safety.
- Dentists. Dental sedation helps patients maintain a calm, restful state during treatment. It involves using a soothing agent to make patients feel calm, relaxed, and at ease during dental procedures. It is a safe and effective method necessary for pain relief and to stop the gag reflex while the dentist works inside the mouth. The dentist or dental nurse can work more quickly and efficiently while the patient is asleep or semiconscious.
- Nurse practitioners. Nurses play various roles, including reassuring and supporting the patients, acting as chaperones, answering any questions they may ask, and keeping detailed notes, such as the patient’s medical and social history. They can assist in sedation and help in emergencies.
- Physician assistants. Physician assistants provide various services, from diagnosing to assisting during surgeries. They must not only differentiate sedation types but be able to determine the needed dosage based on pre-procedure assessment. They also manage patients before, during, and after sedation administration.
Although sedation can be used in dentistry, surgery, or diagnostics, each requires a different level of sedation training. Physicians, dental healthcare specialists, physician assistants, nurse practitioners, and others need specific levels and combinations of sedation training based on their functions and roles.
Advancing Sedation Training Through Innovative Approaches
The future of safe sedation training is shifting from classroom-style instructions to hands-on simulation and innovative practices. This will lead to approaches that offer greater flexibility, cost-effectiveness, and customization. Such a shift from traditional training methods should incorporate patient safety and regulatory standards. Introducing innovation while maintaining competency-based education provides an individualized learning experience that objectively evaluates skills while minimizing costs and disruptions. New ways for advancing in sedation training involve the following innovative approaches.
Simulation-Based Training
Sedation can involve dealing with high-stakes situations and life-threatening events. In these cases, the margin for error is small. However, simulation-based training can serve as a learning tool that supports the development of sedation skills. Trainees enact real-life clinical and sedation events using imitation or replicating situations with potential patients.
Those undergoing training can learn to practice in these lifelike scenarios while gaining hands-on experience. It also allows educators to strategically create training exercises, such as airway management and malignant hyperthermia, in an environment that reduces patient safety concerns and permits repetitive practice. Trainees can improve their situational judgment in real time.
Virtual Reality (VR) Integration
Virtual reality creates a make-believe world through tracking movements and 3D close-up visuals. It gives a real-life feel, just like in simulated training. With VR, educators can create pretend situations that relate to sedating patients. The VR programs can cover sedation methods, handling emergencies, and patient care.
Interdisciplinary Training
Interdisciplinary training is about arranging programs and getting healthcare pros from various fields to work together. It helps them learn more and get better at sedation practices. This wide-ranging collaboration allows for complete patient care and lets medical specialties share their skills.
Exploring Innovation in Sedation Management
During the 1870s, chloral hydrate was first employed as a sleep aid and sedative in Germany. However, chloral hydrate is a toxic substance that has a range of side effects. It can cause skin irritations or stomach discomfort and pain. It sometimes leads to kidney, heart, and liver failure. The 1870s had minimal regulations regarding this matter. Over time, sedation improved in safety. One such example is the European approval of propofol in 1986. It became certified in the USA in 1989. Sedation practices and the technology used in sedation management have developed so much since then, yet they are still progressing.
The evolution of sedation management started in 1995 when the first set of guidelines was published. However, the common belief in the 80s was to make patients adapt to machines. This influence led to deep sedation (DS) and prolonged immobility in many health facilities. However, in the 90s, there was a paradigm shift. Sedation machines and methods would now adapt to the patient’s needs.
The idea of a protocolized sedation took off, with several guidelines published on using midazolam for short-term sedation and lorazepam for long-term sedation. For example, the following protocols and guiding principles became established:
- In the early 2000s, the Richmond Agitation Sedation Scale (RASS) and Sedation Agitation Scale (SAS) were determined to be the most accurate level of arousal assessment tools developed by a multidisciplinary team.
- In 2002, the Clinical Practice Guidelines for the Sustained Use of Sedatives and Analgesics in the Critically Ill Adult (SAG) were published.
- 2013, the Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult ICU Patients (PAD) were published.
Typically, performing RASS takes less than 20 seconds and requires minimal training. Although it has proven highly reliable among multiple healthcare professionals, emerging electroencephalography (EEG) technology can supplement it. EEG innovation in sedation management can enhance patient safety and enable future effective and continuous patient monitoring.
Conclusion
Innovative approaches such as VR integration and simulation-based training are promising. However, these new training modalities need testing and research into their potential. No matter how training occurs, resuscitation equipment and a trained workforce should also be available to handle emergencies.
The medical team performing sedation should have monitoring equipment such as ECG, pulse oximeter, ETCO2, NIBP, and defibrillator, which should be handy in working conditions. One day, EEG technology can also be an option for sedation teams. Healthcare professionals handling sedation should know the latest protocol updates and keep their training abreast.