Is there an app for that? It’s a question no longer reserved for consumers. The entire healthcare experience is changing rapidly for practices, physicians and patients thanks to technology. And this is a very good thing.
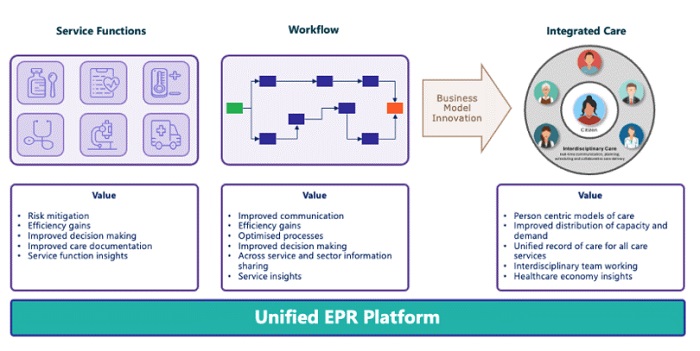
Technology has the potential to democratize access and improve care for all — if we build the right kind of ecosystem for it to thrive.
That means giving innovators the support and visibility they need to bring their solutions to market. It means giving providers seamless access to tools that can assist with everything from patient intake to diagnosis, billing and engagement. And it means giving individuals more control and insight into their own care journeys. When we foster opportunities for collaboration and open up pathways for innovation to scale, we help drive meaningful, lasting transformation in healthcare.
It seems so obvious, doesn’t it? The need for a singular destination to unite an entire ecosystem. To me, this once sounded like a far-off dream. Today, it’s a reality. One only has to know where to look.
Bringing a Vision to Life
The story of healthtech is a story of evolution, much like that of CharmHealth. The company began when I needed access to medical information as a caregiver. At that time, I found very few options — none of them satisfactory. So, I leaned into my tech background to build a platform for parents and caregivers where they could share information about various drugs, their reviews, what worked, and what didn’t work. I designed a space where patients and caregivers could enter their data into a database and track therapeutics and improvements while sharing with others.
Once I had gained some users, I took my burgeoning app to a conference where providers discovered it. They had never seen anything like it and wanted it in their practices. Their feedback and input formed the basis for what is now CharmHealth’s electronic health record (EHR) system. This experience of building something and connecting with others made me realize one thing: If I could create such an application, there must be countless other entrepreneurs doing the same — just waiting to make a difference in healthcare.
So we launched the CharmHealth Innovation Challenge to find out. We invited entrepreneurs, researchers and thought leaders to submit projects addressing specific challenges in healthcare. The types of applications being developed and how they reached and impacted patients and providers were mind-blowing. I wanted everyone to have the ability to discover these wonderful solutions.
Concurrently, CharmHealth was growing significantly. We’d begun working with some truly incredible partners to integrate our respective technologies. Seeing all the positive changes happening when people within the healthtech space collaborate gave rise to a new idea — a home not just for healthtech solutions but also for connections that could enable us to build a better system of care together.
Space for Solutions to Flourish
CharmHealth is based on a simple tenet: Access to quality healthcare should not be a luxury but a fundamental human right. To get there, we made my dream come to life, by launching CharmHealthHub as a destination for anyone seeking or building solutions. It is just as ambitious as it sounds: With CharmHealthHub, we are uniting an entire ecosystem, a vibrant marketplace, to create a healthier, better world for all. More specifically, CharmHealthHub was built with constituents’ unique needs in mind.
Here’s what sets CharmHealthHub apart:
- Equal Access to Innovation: Cutting-edge technologies should not be limited to providers in large health conglomerates. This new tech hub gives all providers equal opportunity to discover the solutions that work best for their needs.
- Support for Startups and Researchers: Innovation should not be stalled by lack of funding or insider connections. Entrepreneurs and researchers building new solutions need a space like CharmHealthHub to launch their inventions, monetize their apps, and easily integrate with the platforms providers rely on.
- Empowered Consumers: Patients are part of the care equation too. CharmHealthHub introduces new technologies they can use to monitor their health and share relevant information with their care team in real time.
- Developer-Friendly Integration: The pathway for creating new solutions should not be so fraught with hurdles that ideas languish by the wayside. On CharmHealthHub, it is easy for developers to gain access to the APIs they need to build applications that seamlessly integrate with the systems used by providers, practices and patients every day.
Whether it’s AI-enabled tools for clinical decision support, workflow-enhancing devices, apps to streamline administrative tasks, or patient engagement solutions, CharmHealthHub is a singular destination where innovation meets integration. And this is just the start.
Who Is CharmHealthHub For?
CharmHealthHub brings together an entire community, including but not limited to:
- Healthtech developers and vendors seeking to build and share apps that enable a frictionless experience for physicians and patients.
- Labs and prescription centers that can be integrated into physicians’ workflows.
- IT consultants or billing/revenue cycle management services.
- System integrators and health IT migration experts.
- Device manufacturers that help providers’ workflows.
- Investors and venture capitalists looking for new investment opportunities.
It also showcases submissions from our Innovation Challenge that have proven to show value to providers and patients. For example, HealMed is transforming mental healthcare with AI, while HireMe Healthcare is reestablishing trust in healthcare hiring to help make healthcare more accessible and affordable for all.
Steps to Better Care
CharmHealthHub can open a whole new world of possibilities for better care, which can be both exciting and overwhelming. Browsing through solutions, for example, can make one feel like there is a “fix” for everything. If you are a provider or run a practice group, don’t try to do it all at once. Pick a select problem you want to solve, engage with vendors to discuss the best way to implement it for your situation, test it, and deploy. This is a repeatable process so that every provider can enhance their standard of care — all through CharmHealthHub.
The marketplace of CharmHealthHub can also help identify some areas where perhaps practices could use some improvement. Read the reviews. Understand how transformative a particular solution has been to someone facing a similar issue. Use the space to connect and learn from one another — as well as to help vendors improve their solutions. Provide feedback and suggest new features. This is how the ecosystem grows in a productive way that can make a deep impact on healthcare systems, practices and procedures. It is beneficial for us all.
At CharmHealth, we believe the future of healthcare is accessible, decentralized and deeply human. This shift is being powered by technologies like telehealth, wearables and integrated apps that make the physician-patient relationship more fruitful, in ways that can improve patient outcomes.
They say that knowledge is power. We are taking that power and combining it with the right amount of care, compassion and innovation for better experiences. We see CharmHealthHub as a stepping stone to a future where quality healthcare isn’t confined by geography, access or privilege and where technology catalyzes a healthier population — one connection at a time.

Pramila Srinivasan, Ph.D., CEO, CharmHealth
Pramila Srinivasan graduated from Purdue University with a Ph.D. in electrical and computer engineering in 1997. She founded MedicalMine Inc in 2007, inspired by a desire to enable medical establishments, large and small, to access cutting-edge technologies to assist in clinical care and documentation. Building on that success, she founded CharmHealth out of a desire to provide superior cloud-based solutions for practice management, clinical care, and patient engagement.
Prior to this, Dr. Srinivasan worked in research and development in areas of multimedia signal processing algorithms and medical data neural network classification, security algorithms, and speech recognition in startup companies that developed technologies for leading consumer electronics products. She also serves as president and founder of The BRAIN Foundation, a California non-profit with the mission to accelerate development of FDA-approved therapeutics to benefit individuals with neurodevelopmental disorders.