The Rise of the Quantified Self: Personal Intelligence in Prevention
For most of medical history, the doctor-patient interaction was defined by the presence of disease. A person would seek medical attention only when symptoms became bothersome, making the healthcare system inherently reactive. However, the emergence of wearable health technology advancing prevention is rewriting this narrative. We are entering an era of “proactive wellness,” where individuals are equipped with laboratory-grade biometric monitoring devices that provide a continuous stream of data on their physiological status. This transition is not just about gadgets; it is a fundamental shift in how we define and maintain human health, moving the focus from the hospital ward to the daily life of the individual.
The power of wearable technology lies in its ability to capture the “in-between” moments the 99% of a person’s life that happens outside the doctor’s office. By tracking metrics such as heart rate variability, sleep architecture, blood oxygen saturation, and even subcutaneous glucose levels, these devices provide a high-definition portrait of a person’s unique biological rhythms. When this data is combined with sophisticated AI health analytics, the result is a powerful tool for the early detection of physiological deterioration, allowing for interventions long before clinical symptoms manifest.
Biometric Monitoring Devices: Beyond Step Counting
The first generation of wearables focused largely on basic activity tracking, such as counting steps or estimating calories burned. While useful for general wellness, these tools were limited in their clinical utility. Today’s wearable health technology advancing prevention is a different breed entirely. We now have wrist-worn devices capable of performing single-lead ECGs, detecting atrial fibrillation, and monitoring for signs of sleep apnea. These are no longer just fitness trackers; they are FDA-cleared medical instruments that provide actionable clinical data.
This level of biometric monitoring is particularly transformative for the prevention of cardiovascular and metabolic diseases. For example, a wearable that detects a gradual increase in resting heart rate and a decrease in heart rate variability can alert a user to the early signs of overtraining, systemic inflammation, or even an impending viral infection. This “early warning system” allows individuals to adjust their behavior through rest, hydration, or seeking early medical advice preventing a minor physiological stressor from becoming a major health event. In this way, digital wellness innovation is turning data into a protective shield.
AI Health Analytics: Decoding the Data Stream
The true value of wearable technology is not found in the raw data itself, but in the insights derived from that data. AI health analytics serve as the interpretive engine that translates millions of data points into a clear picture of health. These algorithms can identify subtle correlations that would be impossible for a human to notice. For instance, an AI might find that a user’s blood pressure tends to spike specifically on Tuesday mornings, correlating with a particular work stressor or a lack of sleep on Monday nights.
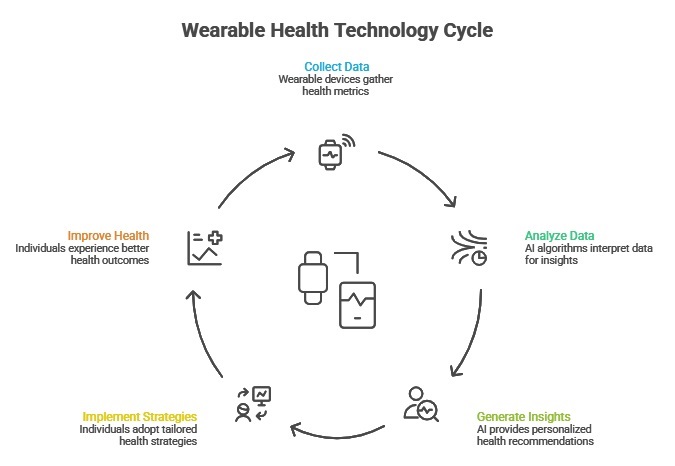 By providing these personalized insights, wearable health technology advancing prevention allows for “n-of-1” medicine an approach where treatment and prevention strategies are tailored to the specific biology and lifestyle of the individual. This is the essence of preventive healthcare: moving away from generic advice like “exercise more” toward specific, data-backed recommendations such as “increase your deep sleep by 20 minutes to improve your glucose metabolism.” This granularity is what makes digital wellness tools so effective at driving long-term behavioral change.
By providing these personalized insights, wearable health technology advancing prevention allows for “n-of-1” medicine an approach where treatment and prevention strategies are tailored to the specific biology and lifestyle of the individual. This is the essence of preventive healthcare: moving away from generic advice like “exercise more” toward specific, data-backed recommendations such as “increase your deep sleep by 20 minutes to improve your glucose metabolism.” This granularity is what makes digital wellness tools so effective at driving long-term behavioral change.
Preventive Healthcare Models and the Clinical Connection
As wearables become more sophisticated, they are being integrated into broader preventive healthcare models. We are moving toward a “collaborative care” system where patients share their wearable data with their primary care physicians. This allows for a more informed and efficient consultation. Instead of the doctor asking, “How have you been feeling for the last six months?” they can open a dashboard and see exactly how the patient’s vitals have trended over that period.
This continuous data flow allows for “micro-interventions.” If a physician sees a patient’s activity levels dropping and their stress markers rising, they can reach out via a secure messaging platform to check in before a clinical problem develops. This proactive outreach is a cornerstone of the next generation of primary care, where the goal is to keep the patient out of the clinic as much as possible. By fostering a constant connection, wearable health technology advancing prevention is strengthening the bond between the individual and their care team, creating a more responsive and resilient health system.
Patient Engagement and the Psychology of Health
One of the most powerful aspects of wearable technology is its ability to increase patient engagement. When a person can see their health data in real-time, they become more invested in their own outcomes. The “gamification” of health using badges, streaks, and community challenges is a powerful tool for motivating consistent healthy behaviors. However, the impact goes deeper than just rewards; it is about building health literacy and a sense of agency.
Wearable health technology advancing prevention provides individuals with the evidence they need to see that their choices matter. Seeing an immediate improvement in sleep quality after a day of increased physical activity or a stress-reduction session provides a powerful positive reinforcement. This sense of control is essential for the management of chronic conditions and the prevention of lifestyle-related diseases. By making the invisible processes of the body visible, these tools are turning wellness into an active, engaging, and personalized journey.
Privacy, Ethics, and the Ownership of Health Data
As we embrace the benefits of wearable health technology advancing prevention, we must also navigate the complex ethical landscape that comes with constant monitoring. The data generated by these devices is incredibly intimate, providing a window into a person’s most private behaviors and physiological states. Consequently, the issues of data ownership, privacy, and security are paramount. Users must have absolute control over who has access to their data and how it is used.
There is also the risk of “biometric anxiety,” where constant monitoring leads to an obsessive focus on data points that may not be clinically significant. It is essential that digital wellness innovation is accompanied by clear guidance on how to interpret data and when to seek professional help. The goal of wearable technology is to support health, not to create a new source of stress. Striking the right balance between awareness and obsession is a key challenge for the developers of these systems.
Future Directions: Towards a Predictive and Personalized Future
The future of wearable health technology advancing prevention is one of increasing integration and sophistication. We are seeing the development of “invisible wearables” sensors embedded in clothing, jewelry, or even as temporary epidermal “tattoos.” These devices will provide even more seamless monitoring without the need for a bulky wrist-worn unit. At the same time, the integration of wearable data with genomic information and environmental sensors will allow for a truly holistic view of health.
We are moving toward a future where “prevention” is not just an occasional check-up, but a continuous, intelligent process that happens in the background of our lives. Through the continued advancement of biometric monitoring and AI health analytics, we are building a world where health is not something we wait to lose, but something we actively and intelligently preserve. The wearable revolution is, at its heart, a human revolution a movement toward a more informed, empowered, and healthy society.


















