The Convergence of Intelligence and Instrumentation in Modern Medicine
The landscape of secondary and tertiary healthcare is currently witnessing a paradigm shift that was once the province of science fiction. The traditional image of a hospital a place of reactive treatment and manual documentation is rapidly fading, replaced by a dynamic, proactive environment where smart medical devices driving hospital innovation act as the central nervous system of the facility. These devices do not merely perform functions; they perceive, analyze, and communicate, creating a tapestry of data that allows clinicians to stay steps ahead of potential complications. This transition is not born of a desire for gadgets, but from a necessity to address the mounting pressures of aging populations, rising costs, and the need for absolute clinical precision.
As these intelligent systems become more deeply embedded in the daily rhythms of clinical care, the very definition of “medical equipment” is being rewritten. We are moving away from isolated units that require constant human oversight toward autonomous and semi-autonomous systems that provide continuous surveillance. This is the bedrock of the modern medical facility, where the integration of advanced sensors and machine learning algorithms ensures that every heartbeat, every breath, and every chemical change in a patient’s body is accounted for and contextualized.
The Architect of the Connected Clinical Environment
At the heart of this revolution lies the concept of connectivity. The implementation of connected healthcare systems has allowed for a level of transparency and fluidity in data management that was previously unattainable. When a ventilator, an infusion pump, and a cardiac monitor are all part of the same digital conversation, the resulting synergy is far greater than the sum of its parts. This interconnectivity ensures that clinical data analytics are fed by a constant stream of high-fidelity information, enabling a more holistic view of the patient’s status.
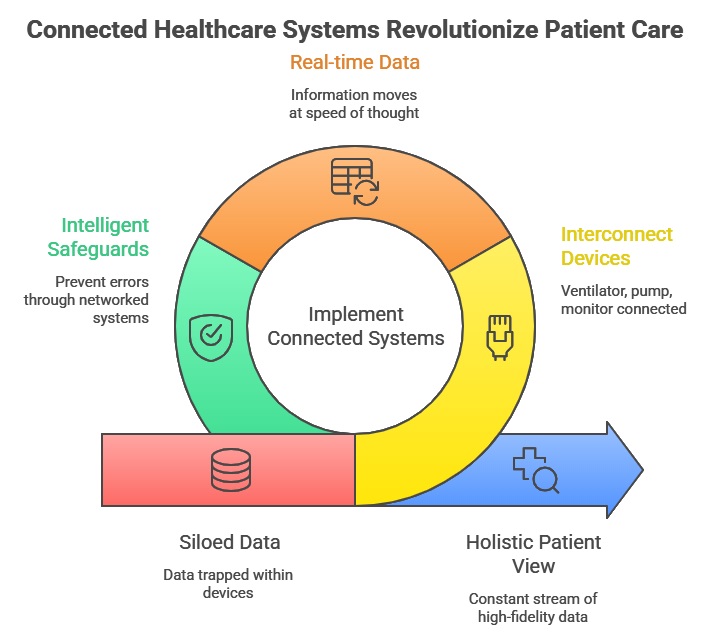 In the past, data was often siloed, trapped within a specific device or written on a physical chart that might not be updated for hours. Today, smart medical devices driving hospital innovation ensure that information moves at the speed of thought. When a smart infusion pump detects a potential dosing error based on the patient’s latest lab results retrieved automatically from the hospital’s central database it can prevent a catastrophic event before it occurs. This is the essence of innovation: the removal of human error through the application of intelligent, networked safeguards.
In the past, data was often siloed, trapped within a specific device or written on a physical chart that might not be updated for hours. Today, smart medical devices driving hospital innovation ensure that information moves at the speed of thought. When a smart infusion pump detects a potential dosing error based on the patient’s latest lab results retrieved automatically from the hospital’s central database it can prevent a catastrophic event before it occurs. This is the essence of innovation: the removal of human error through the application of intelligent, networked safeguards.
The Role of the Internet of Medical Things
The Internet of Medical Things, or IoMT, is the framework that supports this high-level connectivity. By equipping standard medical tools with IoT capabilities, hospitals are transforming every bed, every room, and even the patients themselves into active nodes in a vast information network. IoT medical devices range from smart beds that monitor patient movement to prevent pressure ulcers, to wearable biosensors that track vital signs with laboratory-grade accuracy while the patient is mobile.
These devices provide a granular level of detail that traditional intermittent monitoring could never achieve. Instead of a snapshot of a patient’s health taken every four hours by a nursing team, clinicians now have access to a cinematic view of the patient’s physiological trends. This continuous data stream is vital for early warning systems. In many cases, physiological deterioration begins hours before it becomes clinically obvious to a human observer. Smart medical devices driving hospital innovation leverage this data to trigger alerts that allow for early intervention, significantly reducing the incidence of “code blue” events and unplanned ICU admissions.
Enhancing Clinical Decision Support Through AI
The sheer volume of data generated by an IoMT-enabled hospital would be overwhelming for human staff to process unaided. This is where AI healthcare integration becomes indispensable. Artificial intelligence acts as the interpretive layer that sits atop the hardware. It scans the incoming data for patterns, anomalies, and correlations that might escape the human eye. For instance, an AI-driven monitoring system might notice a subtle, simultaneous change in respiratory rate and oxygen saturation that, when combined with a specific heart rate variability pattern, suggests the early onset of sepsis.
By providing these insights directly to the bedside clinician, these systems function as a force multiplier for the medical staff. They don’t replace the doctor’s judgment; rather, they provide the doctor with a more refined and actionable set of data upon which to base that judgment. This synergy between human expertise and machine intelligence is the primary driver of improved patient outcomes in the modern era.
Operational Efficiency and the Future of Resource Management
Beyond the direct clinical benefits, smart medical devices driving hospital innovation are also reshaping the operational and financial health of medical institutions. Hospitals are notoriously complex environments with massive overhead and intricate logistical challenges. Digital health technology provides the tools to streamline these processes. For example, real-time location systems (RTLS) integrated into medical devices allow staff to locate essential equipment instantly, saving thousands of hours annually that were previously wasted on manual searching.
Furthermore, predictive maintenance powered by internal diagnostics in smart devices can alert technicians to a potential failure before it happens. An MRI machine that can “sense” a cooling system issue and schedule its own repair during off-hours ensures that patient throughput is not interrupted. This level of operational intelligence reduces downtime, extends the lifespan of expensive capital equipment, and ultimately lowers the cost of care delivery.
Privacy, Security, and the Ethical Imperative
As we embrace these technological leaps, the responsibility to protect patient data becomes more acute. The transition to a digital-first hospital environment necessitates robust cybersecurity frameworks. Every connected device is a potential entry point for unauthorized access, making security a core component of the device’s design rather than an afterthought. Manufacturers and hospital IT departments are now working in lockstep to ensure that data-driven clinical decision making does not come at the cost of patient privacy.
Encryption, multi-factor authentication, and blockchain-based data integrity protocols are becoming standard features in the next generation of medical technology. This focus on security is essential for maintaining the trust between patients and the healthcare system. Without a secure foundation, the promise of smart medical devices driving hospital innovation cannot be fully realized.
Sustainable Innovation and Global Health Impact
The final frontier of this movement is its scalability. While the most advanced smart hospitals are currently located in high-income regions, the modular nature of many smart medical devices driving hospital innovation means they can be deployed in resource-limited settings to bridge the gap in care quality. Remote diagnostic tools and AI-enabled screening devices can bring specialist-level care to rural areas where doctors are scarce.
As we look toward the future, the goal is not just to make hospitals “smarter” for the sake of technology, but to make them more effective, more humane, and more accessible. The integration of intelligence into medical devices is the most significant leap forward since the advent of the stethoscope. It represents a commitment to a future where medicine is truly personalized, predictive, and preventative. Through the continued development of these technologies, we are not just changing how we treat disease; we are changing how we value and preserve human life in a digital age.
The journey toward total hospital innovation is ongoing. Each new device and every refined algorithm brings us closer to a healthcare system that works as a cohesive, intelligent whole. By prioritizing the human element within this technological framework, we ensure that the focus remains exactly where it belongs: on the recovery and well-being of the patient.


















