Preoperative risk assessment is critical in ensuring the safety and success of surgical procedures, especially as our elderly population grows and the demand for complex surgeries increases. By 2041, 26% of the UK’s population will be over 65 years old, up from 18% in 2016. Similarly, in the United States, roughly one in six residents were 65 or older in 2020, a substantial increase from less than one in 20 a century earlier.
With an aging demographic increasingly undergoing intricate surgeries, preoperative evaluation is no longer a mere formality but a critical component of comprehensive patient care. Now, a greater number of elderly individuals and those with multiple health problems are subjected to high-risk surgical procedures, which can result in an increased risk of postoperative complications and mortality.
“Major surgery is like running a marathon,” Ben Shelley, Consultant in Cardiothoracic Anaesthesia and Intensive Care and Honorary Professor at the University of Glasgow, said. “It requires your cardiac output to increase hugely in the postoperative period. You’ve got to be able to deliver that. Of the patients who can’t deliver that, we know they are the ones who are at higher risk.”
To gauge a patient’s readiness for surgery, providers often use the patient’s exercise capacity as a proxy measure. However, accurately assessing their physical capabilities can be challenging. Asking patients about their fitness levels can be unreliable, as their recollections are often inaccurate. On the other hand, rigorous laboratory-based physiological testing is effective but expensive, limited in availability, and inaccessible to all patients.
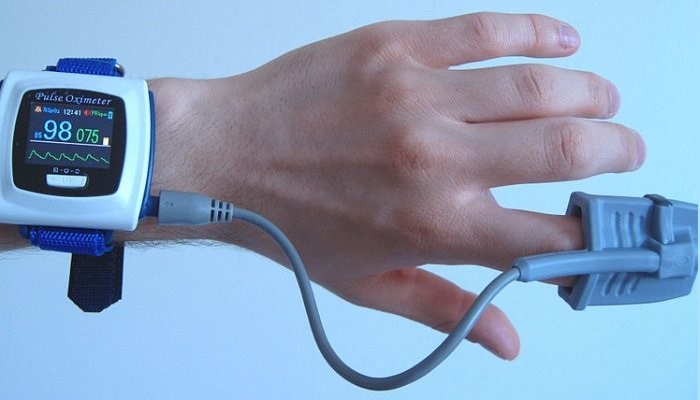
Wearable technology, a focus of Shelley and medical student Jim Luckhurst’s recent research, provides an opportunity to enhance preoperative assessment. Wearable sensors can continuously monitor vital signs like heart rate, blood pressure, and oxygen levels, offering real-time data reflecting a patient’s baseline condition. Leveraging sensors can make preoperative assessments more precise, efficient, and patient-centered, contributing to safer surgeries, improved postoperative outcomes, and increased patient satisfaction.
The importance of preoperative risk assessment
Surgical decision-making is a complex process that involves assessing potential benefits and risks. Informed decisions rely on understanding the patient’s medical history, health status, and the type of surgery. Preoperative risk assessment is conducted to minimize surgical complications, ensure patient safety, and improve outcomes from the moment of decision to operate until well after surgery has been completed.
“The bread and butter of anesthetic preoperative assessment is the assessment of functional capacity and aerobic fitness,” Shelley said. “We’re then able to identify patients at high risk and as a result, tailor perioperative care and monitoring accordingly to mitigate increased risk and improve outcomes.”
The assessment examines the patient’s physical and physiological preparedness for the intended procedure. Various factors collectively influence a patient’s fitness, including cardiovascular health, pulmonary function, nutritional status, frailty, and overall functional capacity.
Traditional methods for assessing patient fitness
Traditionally, preoperative assessment relies on estimating functional capacity through subjective or objective techniques. Subjective tools like the Surgical Outcome Risk Tool (SORT) offer convenience and ease of use, but they also have limitations. The test often fails to comprehensively assess a patient’s physiological readiness for surgery. A clinician’s judgment alone may result in variations in assessments and inconsistencies in risk assessments.
Research has shown that subjective assessment tools may inaccurately predict postoperative outcomes, including mortality and complications. A prospective cohort study that compared subjective assessments with alternative markers of fitness found that subjective assessment tools are unreliable and should be used cautiously.
As a result, healthcare professionals have turned to objective methods for evaluating functional capacity. Cardiopulmonary exercise testing (CPET) has long been considered the gold standard. During CPET, patients must gradually increase exercise intensity until reaching maximal effort. While CPET offers valuable insights into physiological responses to exercise, limitations include cost constraints, patient variability impacting accuracy, and discomfort for some due to its maximal nature.
Submaximal exercise tests and heart rate recovery
For these reasons, researchers have explored submaximal exercise tests (SETs) as more accessible alternatives to CPET. Unlike CPET, SETs involve everyday activities like climbing stairs or walking, making them more feasible and cost-effective. However, SETs still rely on how motivated a patient feels on a given day, which can make the results less dependable. As a result, researchers, including Shelley and Luckhurst, have turned to heart rate recovery as an effective marker of aerobic fitness.
“We’re interested in how your heart rate recovers after exercise,” Shelley said. “If you exercise enough to raise your heart rate, the physiology that drives how it will recover is based on your fitness. Regardless of how much effort you put in or your motivation, intrinsically, your fitness will dictate how your heart rate recovers from exercise. Our focus on heart rate recovery serves as a potential predictor of postoperative outcomes.”
A patient’s heart rate recovery (HRR) has previously been utilized as a prognostic tool in a variety of clinical populations, including healthy individuals, heart failure patients, and those recovering from non-cardiac surgery. In a particular study, researchers explored abnormal heart rate patterns during exercise and recovery in individuals who appeared to be in good health. The results unveiled an association between specific irregularities in heart rate profiles and a heightened risk of sudden death.
Exploring HRR after submaximal exercise
Although there is a growing interest in assessing HRR after submaximal exercise, research in the area remains limited. To make HRR a valuable tool in the perioperative context, a standardized and validated approach is needed.
As a result, Shelley and Luckhurst have explored the feasibility and validity of using HRR measurements after submaximal exercise to assess patient fitness in a perioperative context. The study set out to answer two key questions:
- Feasibility assessment: The study aimed to determine the practicality of measuring HRR in a participant’s home using wearable heart rate sensors, focusing on convenience and applicability.
- Validation of home measurement: The study sought to validate the accuracy and reliability of HRR measurements taken at home by comparing them with those obtained in a controlled hospital setting, ensuring consistent and reliable results.
“The focus of the study revolves around the question — can we do this in a patient’s own home?” Luckhurst said. “Could we measure their heart rate during their day-to-day activities and extract the same information as we would in a hospital setting?”
During the laboratory portion of the study, more than a dozen volunteers underwent a single submaximal exercise test using a stationary bike. Participants were instructed to exercise to a level designed to raise their heart rate to approximately 70% of their maximum. Then, volunteers were asked to stop exercising and their heart rate was recorded for six minutes while they rested.
Following the test at the research facility, participants took home a wearable for three days. The sensors adhere to the skin, enabling uninterrupted heart rate data collection during patients’ routine activities.
During the monitoring period, volunteers were instructed to perform a submaximal exercise of their choice twice a day, aiming to match the exertion level they experienced during the hospital testing. Participants needed to sustain exercise intensity for one minute, followed by a six-minute rest period.
“The patch also has a high-fidelity accelerometer built in, which allows us to know what the patients are up to,” Shelley said. “We need to know when a patient’s at rest to say, ‘Right, they’ve been doing something. Now, they’re at rest.’ By tracking their heart rate during this transition, the accelerometer allows us to map the heart rate against their activity levels.”
Data analysis and results
As they prepare to conduct a patient study, Shelley and Luckhurst’s encouraging outcomes suggest that expanding preoperative assessment beyond the hospital setting could significantly enhance patient care. This, in turn, suggests wearable sensors could become essential tools in preoperative assessments.
“We compared the results obtained from the heart rate patch in a home setting with those from the laboratory, and the findings strongly indicate the feasibility of conducting this outside a hospital environment,” Shelley said.
Discussing the future application, Shelley envisions a scenario where patients are equipped with wearable sensors before surgery. “Going forward, patients coming for surgery could be told, ‘Please wear this sensor for two days before your clinic visit,’’’ he said. “Then, we’ll have all the information we need about you when you arrive at the clinic, eliminating the need for additional tests that consume extra time and effort.”
Looking ahead, their primary focus is on preparing for a patient study. The goal is to evaluate the practicality and efficacy of their approach within a diverse patient population, encompassing individuals with specific medical conditions and a wide range of health profiles.
“If we can conduct this remotely in a patient’s home, it eliminates the need for them to come to the clinic,” Luckhurst said. “It’s convenient for the patient and doesn’t require a lab environment, making it a cost-effective solution. With all the necessary information at hand, we ensure a streamlined and efficient preoperative process.”