Data-Driven Quality Improvement: Using Analytics to Enhance Patient Outcomes
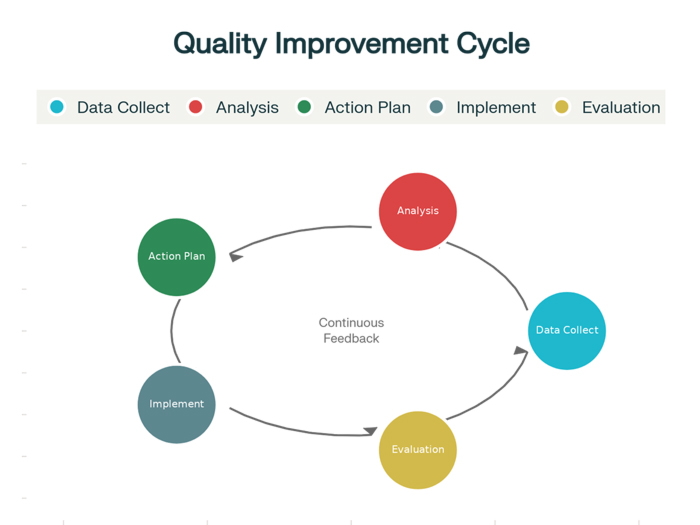
The transformation of healthcare quality improvement from intuition-based approaches to sophisticated data-driven methodologies represents one of the most significant advances in modern healthcare management, fundamentally changing how hospitals identify opportunities, implement improvements, and measure success in patient care delivery. Data driven quality improvement healthcare initiatives leverage the vast amounts of information generated by Electronic Health Records, clinical monitoring systems, patient feedback platforms, and operational databases to create comprehensive insights that guide evidence-based decision making and targeted interventions that directly impact patient outcomes, safety, and satisfaction.
The evolution toward data-driven approaches has been accelerated by advances in healthcare analytics, artificial intelligence, and data visualization technologies that make it possible to process enormous volumes of complex healthcare data and extract actionable insights that were previously hidden within disparate information systems. Modern healthcare organizations generate terabytes of data daily through clinical documentation, diagnostic testing, medication administration, patient monitoring, and operational activities, creating unprecedented opportunities for quality improvement when this information is properly collected, analyzed, and applied to improvement initiatives.
Hospital administrators and quality improvement professionals increasingly recognize that successful implementation of data driven quality improvement healthcare programs requires sophisticated strategies that address data collection, analysis methodologies, visualization techniques, and organizational change management while ensuring that analytical insights translate into practical improvements in clinical practice and patient outcomes. The complexity of healthcare data environments, combined with the critical importance of patient safety and care quality, demands comprehensive approaches that balance analytical rigor with clinical practicality and regulatory compliance requirements.
Foundations of Healthcare Data Analytics
The foundation of effective data driven quality improvement healthcare lies in comprehensive understanding of the diverse data sources, types, and characteristics that define modern healthcare information environments. Healthcare organizations generate data through multiple channels including Electronic Health Records, laboratory information systems, pharmacy management systems, medical imaging platforms, patient monitoring devices, and administrative systems that each contribute unique perspectives on patient care processes and outcomes.
Clinical data encompasses the comprehensive information collected during patient care episodes, including medical histories, diagnostic test results, treatment plans, medication records, vital signs, and clinical observations that provide detailed insights into care quality, safety events, and patient outcomes. This clinical data serves as the primary source for quality improvement analytics because it directly reflects the care processes and results that quality initiatives seek to improve.
Operational data includes information about hospital processes, resource utilization, workflow efficiency, and performance metrics that influence the ability to deliver high-quality care consistently. This operational data helps identify bottlenecks, inefficiencies, and resource constraints that may impact care quality while providing insights for process improvement and resource optimization initiatives.
Patient-reported outcome measures and satisfaction data provide critical perspectives on care quality from the patient viewpoint, capturing information about symptoms, functional status, quality of life, and care experiences that may not be reflected in traditional clinical measures. This patient-centered data helps ensure that quality improvement efforts address outcomes that matter most to patients while providing balanced perspectives on care effectiveness.
The integration of diverse data sources presents both opportunities and challenges for healthcare analytics because different systems often use varying data formats, coding standards, and documentation practices that must be harmonized to create comprehensive analytical datasets. Successful data integration requires sophisticated approaches to data standardization, quality assessment, and validation that ensure analytical results are accurate, reliable, and clinically meaningful.
Analytics Methodologies and Statistical Approaches
Effective data driven quality improvement healthcare requires sophisticated analytical methodologies that can extract meaningful insights from complex healthcare datasets while addressing the unique characteristics and challenges associated with medical data analysis. These methodologies must account for factors such as data completeness, temporal relationships, confounding variables, and clinical significance while providing actionable insights that support practical improvement initiatives.
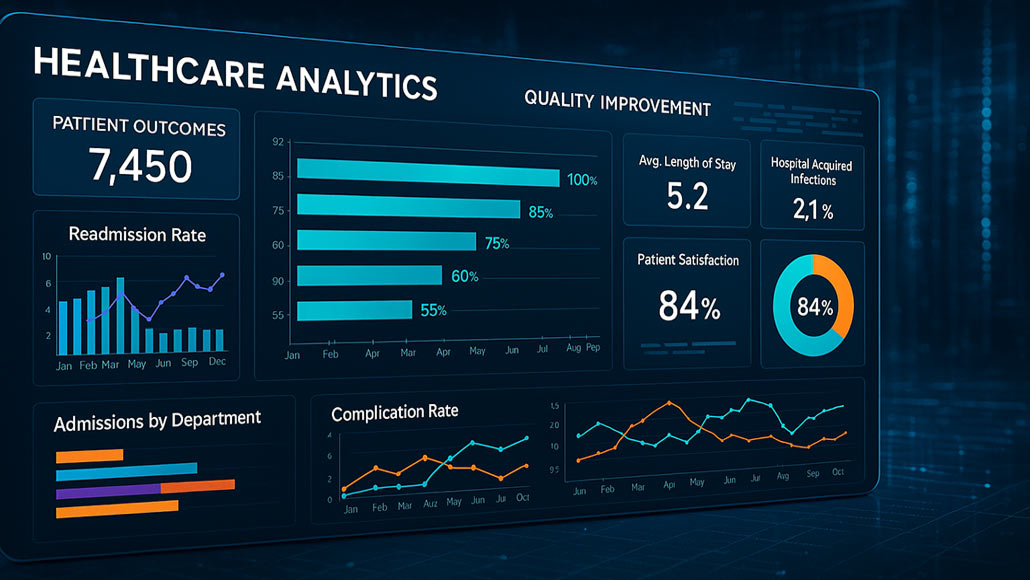
Descriptive analytics provide fundamental insights into current performance by summarizing historical data, identifying trends, and establishing baseline measurements that serve as starting points for quality improvement efforts. These analytical approaches include statistical summaries, trend analysis, benchmarking comparisons, and performance dashboards that help healthcare organizations understand their current quality performance while identifying areas requiring attention or improvement.
Predictive analytics leverage historical data patterns to forecast future outcomes, identify patients at risk for adverse events, and anticipate quality problems before they occur. These approaches include machine learning algorithms, risk prediction models, and early warning systems that enable healthcare organizations to implement proactive interventions that prevent quality issues rather than responding to problems after they have already impacted patient care.
Diagnostic analytics investigate the root causes of quality problems by examining relationships between different variables, identifying contributing factors, and understanding the mechanisms that lead to adverse outcomes or performance gaps. These analytical approaches help healthcare organizations move beyond symptom treatment to address underlying causes that drive quality issues while ensuring that improvement interventions target the most significant contributing factors.
Prescriptive analytics recommend specific actions and interventions based on analytical insights while considering constraints, resources, and potential outcomes associated with different improvement strategies. These advanced analytical approaches combine multiple data sources and analytical techniques to provide actionable recommendations that guide quality improvement decision making while optimizing the likelihood of successful outcomes.
Quality Metrics and Performance Indicators
The selection and definition of appropriate quality metrics represents a critical component of data driven quality improvement healthcare because these measures determine what aspects of care quality are monitored, analyzed, and targeted for improvement. Effective quality metrics must balance comprehensiveness with practicality while addressing clinical outcomes, patient safety, care processes, and patient experiences that collectively define healthcare quality.
Clinical outcome metrics focus on the results of medical care including mortality rates, complication rates, infection rates, readmission rates, and functional status improvements that directly reflect the effectiveness of clinical interventions and care processes. These outcome measures provide essential evidence of quality performance while serving as ultimate targets for improvement initiatives that seek to enhance patient health and well-being.
Process quality indicators measure adherence to evidence-based care protocols, clinical guidelines, and best practices that have been demonstrated to improve patient outcomes when implemented consistently. These process measures include medication administration accuracy, documentation completeness, care coordination effectiveness, and protocol compliance rates that influence the likelihood of achieving desired clinical outcomes.
Patient safety metrics specifically focus on adverse events, near misses, and safety-related incidents that could harm patients or compromise care quality. These safety indicators include medication errors, hospital-acquired infections, patient falls, surgical complications, and other events that represent failures in safety systems and processes that protect patients from harm.
Patient experience measures capture patient perceptions, satisfaction levels, and reported experiences with healthcare services including communication quality, care coordination, respect for preferences, and overall satisfaction with care received. These patient-centered metrics ensure that quality improvement efforts address aspects of care that matter most to patients while providing balanced perspectives on care quality beyond clinical measures alone.
Data Collection and Management Strategies
Successful data driven quality improvement healthcare requires robust data collection and management strategies that ensure information quality, accessibility, and usability for analytical purposes while maintaining patient privacy and regulatory compliance. These strategies must address data collection processes, storage systems, quality assurance procedures, and governance frameworks that support reliable and effective quality improvement analytics.
Automated data collection systems leverage Electronic Health Records, medical devices, and clinical information systems to capture quality-related data continuously and consistently without requiring additional manual documentation from healthcare providers. These automated approaches improve data completeness and accuracy while reducing the burden on clinical staff while ensuring that quality metrics are based on comprehensive and reliable information.
Data quality assurance processes establish systematic approaches for identifying and correcting data errors, inconsistencies, and omissions that could compromise analytical results and quality improvement decisions. These processes include data validation rules, automated quality checks, regular audits, and correction procedures that ensure analytical datasets meet standards for accuracy, completeness, and reliability necessary for effective quality improvement.
Data governance frameworks establish policies, procedures, and oversight mechanisms that ensure appropriate access, use, and protection of healthcare data used for quality improvement purposes while maintaining compliance with privacy regulations and ethical standards. These governance structures address data access controls, usage policies, privacy protections, and accountability mechanisms that enable effective quality improvement while protecting patient information.
Real-time data integration capabilities enable healthcare organizations to access current information for quality monitoring and immediate intervention when quality issues are identified. These capabilities include data streaming technologies, real-time dashboards, and automated alerting systems that provide timely information for quality improvement while enabling rapid response to emerging quality concerns.
Analytical Tools and Technology Platforms
The effectiveness of data driven quality improvement healthcare depends heavily on analytical tools and technology platforms that can process large volumes of healthcare data, perform sophisticated analyses, and present results in formats that support decision making and action taking by healthcare professionals. These technology solutions must balance analytical power with usability while providing the performance, security, and integration capabilities necessary for healthcare environments.
Business intelligence platforms provide comprehensive analytical capabilities including data integration, statistical analysis, visualization, and reporting functions that support various aspects of quality improvement analytics. These platforms enable healthcare organizations to combine data from multiple sources, perform complex analyses, and create interactive dashboards and reports that make analytical insights accessible to different user groups with varying technical expertise.
Statistical analysis software offers specialized capabilities for advanced analytical techniques including predictive modeling, risk adjustment, outcome analysis, and comparative effectiveness research that support sophisticated quality improvement initiatives. These tools provide the statistical rigor necessary for healthcare analytics while offering the flexibility to address diverse analytical requirements and research questions that arise in quality improvement work.
Visualization and dashboard technologies translate complex analytical results into intuitive visual formats that enable healthcare professionals to understand quality performance, identify trends, and recognize opportunities for improvement quickly and effectively. These visualization tools should provide interactive capabilities that enable users to explore data, drill down into details, and customize views based on their specific roles and responsibilities.
Cloud-based analytics platforms offer scalability, flexibility, and cost-effectiveness advantages for healthcare organizations seeking to implement sophisticated quality improvement analytics without substantial infrastructure investments. These platforms must address healthcare-specific requirements for security, compliance, and integration while providing the analytical capabilities and performance necessary for effective quality improvement programs.
Implementation Strategies and Change Management
The successful implementation of data driven quality improvement healthcare requires comprehensive strategies that address not only technical and analytical considerations but also organizational change management, workflow integration, and cultural transformation necessary for widespread adoption and sustained success. These implementation strategies must balance analytical sophistication with practical usability while ensuring that data-driven approaches enhance rather than complicate existing quality improvement processes.
Stakeholder engagement throughout the implementation process ensures that quality improvement analytics address the needs and priorities of diverse user groups including physicians, nurses, quality professionals, administrators, and other healthcare team members who will utilize analytical insights in their work. Early involvement of these stakeholders helps identify requirements, address concerns, and build support for data-driven approaches while ensuring that analytical solutions align with actual workflow needs and priorities.
Training and education programs enable healthcare professionals to develop the skills and knowledge necessary for effectively utilizing quality improvement analytics while building confidence in data-driven decision making. These programs should address both technical skills for using analytical tools and conceptual understanding of quality improvement methodologies while providing practical experience with real-world applications and case studies.
Workflow integration strategies ensure that quality improvement analytics become embedded in routine operational processes rather than remaining separate analytical activities that compete for attention and resources. These integration approaches should identify natural connection points between analytical insights and existing quality improvement workflows while minimizing disruption to established processes and procedures.
Performance monitoring and feedback systems track the adoption and impact of data-driven quality improvement initiatives while identifying opportunities for optimization and refinement. These monitoring systems should measure both usage metrics for analytical tools and improvement outcomes resulting from data-driven interventions while providing feedback that guides continued development and enhancement of quality improvement analytics programs.
Measuring Impact and Continuous Improvement
The long-term success of data driven quality improvement healthcare initiatives depends on systematic approaches to measuring impact, demonstrating value, and continuously refining analytical approaches based on experience and changing requirements. These measurement and improvement processes must address both the effectiveness of analytical methods and the clinical outcomes achieved through data-driven quality improvement while providing evidence that justifies continued investment and expansion of analytics capabilities.
Outcome measurement frameworks establish systematic approaches for tracking the clinical, operational, and financial impacts of data-driven quality improvement initiatives while providing evidence of program effectiveness and return on investment. These frameworks should include both short-term process improvements and long-term outcome enhancements while accounting for confounding factors and alternative explanations for observed changes.
Benchmarking and comparative analysis enable healthcare organizations to assess their quality improvement analytics performance against industry standards, best practices, and peer organizations while identifying opportunities for enhancement and optimization. These comparative approaches provide context for performance evaluation while highlighting successful strategies and approaches that can be adopted or adapted for local implementation.
Continuous improvement processes for quality improvement analytics ensure that analytical methods, tools, and approaches evolve based on experience, feedback, and changing requirements while maintaining focus on practical application and clinical value. These improvement processes should include regular review cycles, user feedback collection, and systematic updates to analytical approaches based on lessons learned and emerging best practices.
Innovation and advancement strategies help healthcare organizations stay current with evolving analytical technologies, methodologies, and applications while identifying opportunities to enhance their quality improvement capabilities through adoption of new approaches and technologies. These strategies should balance proven methods with experimental approaches while ensuring that innovation efforts align with organizational priorities and resource constraints.
The path forward for data driven quality improvement healthcare requires sustained commitment to comprehensive analytical programs that combine sophisticated technology capabilities with practical application strategies and organizational change management while maintaining focus on improved patient outcomes and care quality. Organizations that successfully implement these approaches achieve significant advantages in quality performance while building capabilities that support continued improvement and innovation in patient care delivery.