Leading Digital Change: A Hospital Executive’s Guide to Successful Technology Transformation
The imperative for digital transformation in healthcare has evolved from an optional strategic initiative to an existential necessity for hospital survival and success in an increasingly competitive and technology-driven healthcare landscape. Leading digital change hospital executives face unprecedented challenges as they navigate complex organizational transformations that touch every aspect of healthcare delivery, from clinical workflows and patient engagement to operational efficiency and financial performance. The scope and scale of digital transformation in healthcare extends far beyond implementing new technologies to encompass fundamental changes in organizational culture, professional practices, and patient care models that require sophisticated leadership approaches and change management strategies.
Hospital executives today must orchestrate digital transformations while maintaining operational continuity, ensuring patient safety, complying with regulatory requirements, and managing financial constraints that limit their ability to invest in comprehensive technology upgrades. The complexity of these challenges is compounded by the reality that healthcare organizations typically include diverse stakeholder groups with varying levels of technology comfort, different professional priorities, and sometimes conflicting perspectives on the value and risks associated with digital innovation.
The stakes for successful digital transformation have never been higher, as healthcare organizations that fail to adapt risk losing competitive positioning, experiencing operational inefficiencies, and struggling to meet evolving patient expectations for convenient, accessible, and personalized care experiences. Conversely, organizations that successfully navigate digital transformation often achieve significant advantages including improved clinical outcomes, enhanced operational efficiency, increased patient satisfaction, and stronger financial performance that positions them for long-term success in the evolving healthcare marketplace.
Understanding the Digital Transformation Landscape
Digital transformation in healthcare encompasses a comprehensive reimagining of how healthcare organizations deliver care, engage with patients, manage operations, and create value for stakeholders through the strategic integration of digital technologies and data-driven approaches. This transformation extends far beyond simple technology adoption to include fundamental changes in organizational structure, clinical workflows, patient engagement models, and business processes that leverage digital capabilities to achieve strategic objectives.
The current healthcare digital transformation landscape reflects rapid acceleration driven by factors including the COVID-19 pandemic, evolving patient expectations, regulatory changes, competitive pressures, and advancing technology capabilities that create both opportunities and challenges for hospital executives. Organizations across the healthcare spectrum are investing heavily in digital initiatives including Electronic Health Record optimization, telemedicine platforms, artificial intelligence applications, and patient engagement tools while grappling with integration challenges, workflow disruptions, and change management complexities.
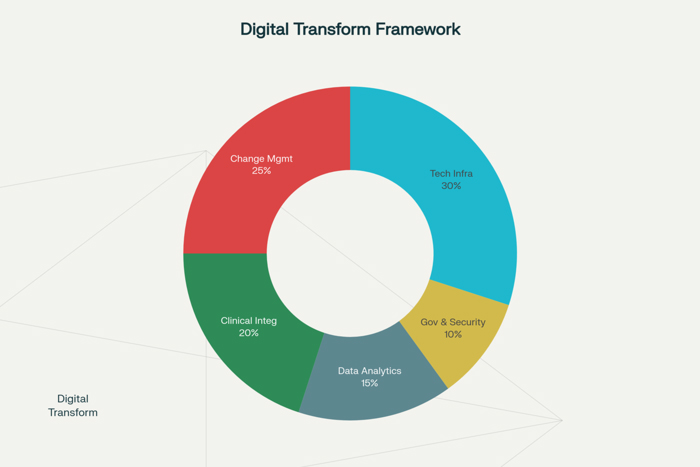
Leading digital change hospital executives must recognize that successful transformation requires holistic approaches that address technology infrastructure, organizational culture, clinical practices, and operational processes simultaneously while maintaining focus on patient care quality and safety. The interconnected nature of healthcare operations means that digital changes in one area often create ripple effects throughout the organization, requiring comprehensive planning and coordination to ensure that transformation initiatives enhance rather than complicate overall organizational performance.
The pace of digital change in healthcare continues accelerating as new technologies emerge, patient expectations evolve, and competitive pressures intensify. Hospital executives must develop strategic frameworks that enable their organizations to adapt continuously to changing conditions while building capabilities that support sustained innovation and improvement over time.
Strategic Vision and Leadership Framework
Effective digital transformation begins with clear strategic vision that articulates the desired future state of the organization while providing direction and motivation for change initiatives. Leading digital change hospital executives must develop comprehensive visions that address clinical care improvements, operational efficiency gains, patient experience enhancements, and competitive positioning while ensuring alignment with organizational mission, values, and strategic objectives.
The development of strategic vision for digital transformation requires deep understanding of current organizational capabilities, market conditions, competitive landscape, and stakeholder needs that influence the direction and priorities for change initiatives. This vision should address both immediate improvement opportunities and long-term transformation goals while providing flexibility for adapting to changing conditions and emerging opportunities.
Leadership framework development becomes essential for hospital executives seeking to guide digital transformation effectively because successful change requires coordinated action across multiple organizational levels and functional areas. These frameworks should establish clear governance structures, decision-making processes, communication protocols, and accountability mechanisms that ensure transformation initiatives receive appropriate leadership support and oversight.
Executive sponsorship and commitment represent critical success factors for digital transformation because organizational change efforts require sustained leadership support to overcome resistance, allocate resources, and maintain momentum through inevitable challenges and setbacks. Hospital executives must demonstrate visible commitment to digital transformation while providing the resources, authority, and political support necessary for successful implementation.
Change leadership competencies for digital transformation differ from traditional management skills because leading digital change requires abilities to navigate ambiguity, manage complexity, facilitate collaboration, and inspire innovation while maintaining operational stability and clinical quality. Hospital executives must develop or acquire these competencies while building leadership teams that can support transformation initiatives effectively.
Stakeholder Engagement and Change Management
Successful digital transformation in healthcare requires comprehensive stakeholder engagement strategies that address the diverse needs, concerns, and perspectives of clinical staff, administrative personnel, patients, and external partners who will be affected by change initiatives. Leading digital change hospital executives must develop sophisticated approaches to stakeholder communication, involvement, and support that build consensus and commitment while addressing resistance and concerns proactively.
Clinical staff engagement represents one of the most critical aspects of healthcare digital transformation because physicians, nurses, and other clinical professionals ultimately determine whether new technologies and processes are adopted effectively in patient care settings. These professionals bring deep expertise in clinical workflows, patient safety requirements, and care quality standards that must inform digital transformation planning while their buy-in and participation are essential for successful implementation.
The challenge of managing clinical resistance to digital change requires understanding the underlying concerns that drive opposition including fears about patient safety, workflow disruption, increased workload, and loss of professional autonomy. Hospital executives must address these concerns through transparent communication, meaningful involvement in planning processes, comprehensive training programs, and demonstration of tangible benefits that align with clinical values and priorities.
Administrative stakeholder engagement involves coordinating with department leaders, middle managers, and support staff who play crucial roles in implementing and sustaining digital transformation initiatives. These stakeholders often serve as change champions or barriers depending on how well transformation initiatives are communicated, planned, and supported throughout the organization.
Patient and family involvement in digital transformation planning helps ensure that technology changes enhance rather than complicate patient experiences while addressing concerns about privacy, accessibility, and care quality that could impact patient satisfaction and engagement. Patient feedback and involvement can provide valuable insights for optimizing digital solutions while building support for changes that may affect how patients interact with healthcare services.
Technology Architecture and Integration Strategy
Digital transformation success depends heavily on robust technology architecture that can support current operational needs while providing scalability and flexibility for future growth and innovation. Leading digital change hospital executives must develop comprehensive technology strategies that address infrastructure requirements, integration challenges, security considerations, and performance expectations while ensuring that technology investments align with strategic objectives and deliver measurable value.
Enterprise architecture planning becomes essential for healthcare organizations undertaking digital transformation because the complexity of healthcare technology environments requires systematic approaches to integration, interoperability, and data management. These architectures should address Electronic Health Record systems, clinical applications, administrative platforms, and emerging technologies while ensuring seamless data flow and consistent user experiences across all systems.
Integration challenges in healthcare technology environments often prove more complex than in other industries because healthcare organizations typically operate legacy systems that were not designed for extensive integration while maintaining strict requirements for patient safety, data security, and regulatory compliance. Successful integration strategies must address these challenges while minimizing disruption to clinical workflows and patient care activities.
Cloud computing strategies enable healthcare organizations to achieve greater flexibility, scalability, and cost-effectiveness in their technology infrastructures while supporting digital transformation initiatives. However, cloud adoption in healthcare requires careful consideration of data security, regulatory compliance, performance requirements, and integration needs that may differ from cloud implementations in other industries.
Cybersecurity considerations become increasingly important as digital transformation expands the attack surface and creates new vulnerabilities that could compromise patient data or disrupt clinical operations. Hospital executives must ensure that cybersecurity measures keep pace with digital transformation initiatives while balancing security requirements with operational efficiency and user accessibility needs.
Implementation Planning and Project Management
Successful digital transformation requires sophisticated project management approaches that can coordinate multiple simultaneous initiatives while managing interdependencies, resource constraints, and timeline pressures that characterize complex organizational change efforts. Leading digital change hospital executives must establish project management frameworks that ensure transformation initiatives are delivered on time, within budget, and with expected benefits while minimizing disruption to ongoing operations.
Phased implementation strategies enable healthcare organizations to manage the complexity and risk associated with large-scale digital transformation by breaking comprehensive changes into manageable segments that can be implemented, tested, and optimized before proceeding to subsequent phases. These strategies should prioritize high-impact, low-risk initiatives early in the transformation process to build momentum and demonstrate value while gradually tackling more complex and disruptive changes.
Resource allocation and capacity management become critical considerations for digital transformation because healthcare organizations must balance transformation investments with ongoing operational requirements while ensuring that staff members have the time, training, and support necessary to adapt to new technologies and processes. Effective resource management requires careful planning and coordination to avoid overwhelming staff or compromising patient care during transition periods.
Risk management for digital transformation initiatives must address both technical risks related to technology implementation and organizational risks related to change management, workflow disruption, and staff resistance. Comprehensive risk management plans should identify potential issues, establish mitigation strategies, and create contingency plans that enable organizations to respond effectively to challenges and setbacks.
Quality assurance processes for digital transformation ensure that new technologies and processes meet performance, safety, and compliance requirements before being deployed in clinical environments. These processes should include testing protocols, validation procedures, and acceptance criteria that verify technology functionality while ensuring that changes enhance rather than compromise care quality and patient safety.
Cultural Transformation and Organizational Development
Digital transformation in healthcare requires fundamental cultural changes that support innovation, collaboration, and continuous learning while maintaining the patient-centered values and safety focus that define healthcare organizations. Leading digital change hospital executives must actively cultivate organizational cultures that embrace technology adoption, encourage experimentation, and reward continuous improvement while preserving the professional traditions and ethical commitments that define healthcare practice.
Innovation culture development involves creating organizational environments where staff members feel empowered to suggest improvements, experiment with new approaches, and learn from both successes and failures without fear of punishment or retribution. These cultures encourage creative problem-solving and continuous improvement while maintaining appropriate controls and oversight to ensure patient safety and quality care.
Learning organization principles become particularly relevant for healthcare digital transformation because the pace of technological change requires continuous skill development and knowledge updating among staff members at all organizational levels. Organizations must establish learning and development programs that keep pace with technology evolution while providing practical training that enables staff to utilize new capabilities effectively.
Collaboration enhancement through digital transformation involves leveraging technology to improve communication, coordination, and teamwork among healthcare professionals while breaking down silos that can impede effective care delivery. Digital collaboration tools should enhance rather than complicate interprofessional communication while providing the documentation and coordination capabilities necessary for complex patient care.
Performance measurement and feedback systems enable organizations to track progress toward cultural transformation goals while identifying areas requiring additional attention or support. These systems should measure both quantitative indicators such as technology adoption rates and qualitative factors such as staff satisfaction, engagement levels, and perceived organizational support for innovation and change.
Financial Management and Return on Investment
Digital transformation initiatives require substantial financial investments that must be justified through demonstrable returns in improved efficiency, enhanced quality, reduced costs, or increased revenue. Leading digital change hospital executives must develop sophisticated approaches to financial planning, budgeting, and return on investment analysis that ensure transformation investments deliver expected value while maintaining fiscal responsibility and organizational sustainability.
Business case development for digital transformation requires comprehensive analysis of costs, benefits, risks, and alternatives that provide stakeholders with clear understanding of the financial implications and expected returns from technology investments. These business cases should address both direct financial impacts and indirect benefits such as improved patient satisfaction, enhanced staff productivity, and competitive positioning that contribute to long-term organizational success.
Cost-benefit analysis for healthcare digital transformation presents unique challenges because many benefits such as improved patient outcomes, enhanced safety, and better care coordination are difficult to quantify in financial terms while implementation costs are often more easily measured and immediate. Effective analysis approaches must capture both tangible and intangible benefits while providing realistic assessments of implementation costs and timelines.
Return on investment measurement for digital transformation requires sophisticated metrics and analysis frameworks that track both short-term efficiency gains and long-term strategic benefits while accounting for the extended timeframes often required for healthcare technology implementations to achieve full value. These measurements should include clinical outcome improvements, operational efficiency gains, and financial performance enhancements that justify continued investment in digital initiatives.
Ongoing financial monitoring and optimization ensure that digital transformation investments continue delivering expected value while identifying opportunities for additional improvements or cost reductions. This monitoring should include regular performance reviews, cost analysis updates, and benefit realization assessments that guide continued investment decisions and optimization efforts.
Sustaining Change and Continuous Improvement
The long-term success of digital transformation depends on organizations’ ability to sustain changes, adapt to evolving conditions, and continue improving their digital capabilities over time. Leading digital change hospital executives must establish governance structures, processes, and cultural norms that support continuous innovation and improvement while maintaining the gains achieved through initial transformation efforts.
Change sustainability requires embedding new technologies, processes, and behaviors into organizational culture and operations so deeply that they become standard practice rather than temporary modifications. This sustainability involves updating policies and procedures, modifying training programs, adjusting performance metrics, and aligning incentive systems to support and reinforce desired changes.
Continuous improvement frameworks enable healthcare organizations to build upon initial digital transformation successes while adapting to changing technology capabilities, patient needs, and market conditions. These frameworks should include regular assessment processes, improvement identification mechanisms, and implementation procedures that ensure organizations continue evolving and advancing their digital capabilities.
Innovation pipeline development helps healthcare organizations maintain momentum for digital transformation by identifying emerging technologies, evaluating potential applications, and planning future implementation initiatives. This pipeline should balance proven technologies with experimental approaches while ensuring that innovation efforts align with strategic objectives and operational capabilities.
Knowledge management and organizational learning systems capture insights, lessons learned, and best practices from digital transformation initiatives while making this knowledge available to support future improvement efforts. These systems should document both successes and failures while providing practical guidance for ongoing digital transformation activities.
The journey of leading digital change hospital executives requires sustained commitment to comprehensive transformation that addresses technology, processes, culture, and leadership while maintaining focus on improved patient outcomes and organizational effectiveness. Success in this endeavor demands sophisticated understanding of change management principles, technology capabilities, healthcare operations, and leadership practices that enable organizations to navigate complex transformations while achieving their strategic objectives and serving their communities effectively.


















