As consumers grow increasingly tech savvy, expectations for e-health services become increasingly pressing. Providers need to be confident that their patients can be accurately identified at all points of service and that information is being effectively shared across systems.
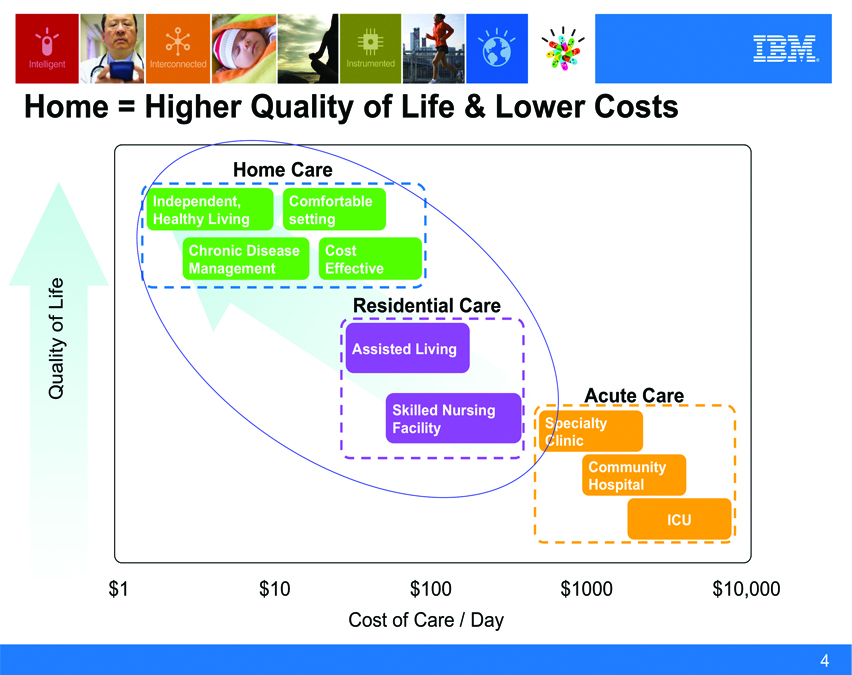
Aging populations, increase in chronic illnesses, pandemic diseases, healthcare provider shortages, and rapidly escalating costs are being seen in all corners of the world.
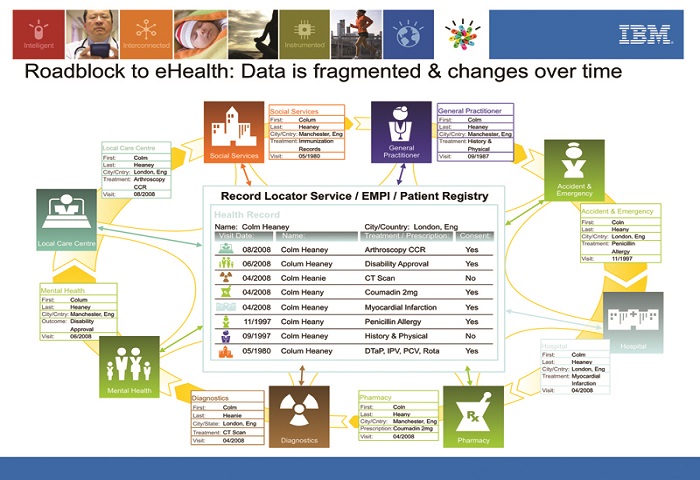
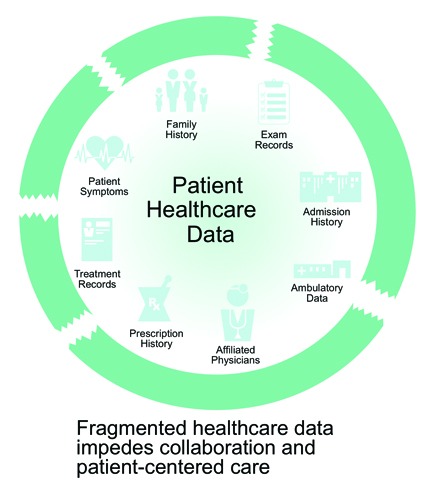
For decades, countries have taken a “siloed” approach to healthcare delivery and the associated data. As a result, valuable clinical data is not always available to promote better, more cost-effective care and deliver valuable insights. However, electronic medical records (EMRs)—that enable the tracking of symptoms, appointments, and treatment plans and provide records for audit—are now universally recognized as essential for patient-centered, connected care. With EMRs, providers can manage clinical documentation, administer tests and review image results electronically, and adopt computerized physician order entry.
Last year Singapore began implementation of its national electronic health record (EHR) system, which allows for the exchange of various types of clinical information among health providers in a single patient view. This will improve disease management and lower costs by eliminating redundant tests and reducing the potential for medication errors.
Once systems like these are operational, data can be harvested for analytics, thus producing valuable information for improving individual and population health. Improved access to information also supports critical decision making and can help healthcare organizations proactively identify ways to enhance operations and support collaboration on improved care models and practices.
Interoperability and the development of related standards that allow for the safe exchange of data have become integral to every technology used to address health goals, as the following three successful areas demonstrate:
• Diagnostic imaging’s impact on patient’s safety and cost has made radiology information systems/picture archiving communications systems (RIS/PACs) and the facilitation of image sharing a high priority across the world. A key proof point for HIE’s return on investment, RIS/PACS save time, eliminate the need for retesting, and can reduce costs and improve patient safety.
• Telemedicine initiatives expand services and the efficient use of resources across broad geographical areas—particularly rural areas with few medical professionals. Telemedicine is enhanced through electronic health information, such as the imaging provided by RIS/PACs.
• E-prescribing increases patient’s safety by reducing errors in prescribing and facilitating medication reconciliation. Thus, preventing adverse drug interactions.
Data can be harvested for analytics, thus producing valuable information for the improvement of individual and population health.
Best Practices and Success Factors
While no single formula for HIE success exists, several valuable lessons can be shared.
A definitive plan or framework – Healthcare transformation may require policy development, technology framework, and/or an overarching strategic plan. Addressing these before spending precious financial resources ensures jurisdictions are “building” to a demonstrable, quantifiable vision to achieve interoperability.
Canada implemented components of this with the organization and funding of Canada Health Infoway and the development of the Health Information Access Layer as part of its national blueprint. Monies were paid to the provinces after they demonstrated compliance and achieved project milestones.
Additionally, over a decade ago, Hong Kong embarked on a clinical system initiative with a plan to enable data sharing across its medical infrastructure. Today, its Electronic Patient Record Sharing Pilot Project (PPI-ePR) is establishing a web-based system to integrate patients’ information in real time to be shared among clinics and public and private hospitals. Registered patients are assigned a personal identification number and, upon providing consent, can use the secure platform to give participating private healthcare providers access to their individual electronic patient records (ePRs).
Multi-stakeholder participation – Physicians, nurses, health professionals, and even consumers (patients) are all vital participants in healthcare transformation and redesign. Diverse stakeholder participation in the planning, development, and execution of healthcare transformation and HIE is critical, even in countries with a publicly funded health system.
With regard to data exchange, stakeholders may need to implement a required response time to ensure user satisfaction or address workflow changes to extract maximum value from shared data. When these requirements are taken into consideration from the outset, stakeholders are more likely to embrace initiatives specifically created with their needs at top of mind.
Working towards a vision and measurable outcomes – Healthcare permeates every nation’s economy, growth, tax structure, and citizen productivity. The need to consistently advance healthcare delivery means we can no longer afford to waste time on pilot programs that lack a clearly defined, aggressive end goal or metrics to demonstrate success. Programs for telemedicine, electronic records exchange, or other initiatives must be guided by a broader vision of the ideal outcome than making it “work.”
Clarity of purpose also helps dictate which technology can best be utilized. The European Union is moving to this approach, particularly for funding countries with failing economies. Bailouts require dramatic changes in healthcare execution and a clear vision of the expected impact on local healthcare.
Transparency – When viewpoints are publicly shared and considered, consumers can support policies and technologies for electronic data capture and data sharing, providers can plan their technology needs, and governments can balance the needs of the diverse constituency that must support healthcare transformation.
The United States has done a commendable job of achieving transparency through efforts by the Office of the National Coordinator for Health Information Technology (ONC) in public committee and workgroup meetings, open comment periods, and formal public hearings on key topics. Every gathering has a segment devoted to open public comment.
If all nations take a holistic look at their current practices and work to identify areas where new processes and technologies can be introduced to help streamline delivery and quality of care, we will see today’s complex healthcare challenges become increasingly more manageable in the journey toward connected and personalized patient care. Countries, regions, and jurisdictions that embrace e-health and learn from others will succeed in healthcare transformation at all levels.
IBM’s Smarter Healthcare Strategy
The journey to sustainable healthcare systems starts with a smarter approach to information sharing. IBM Information Management solutions for healthcare deliver master data management (MDM) capabilities that help stakeholders to connect and share clinical information accurately, securely and cost-effectively. IBM Initiate Patient and IBM Initiate Provider are a trusted foundation for information sharing around the globe; they help healthcare organizations improve collaboration to increase quality of care, streamline compliance and increase patient and provider satisfaction. For more information visit www.IBM.com/Infosphere/healthcare-providers.