Hardly a day goes by without a story coming to light about promising new research into the application of artificial intelligence (AI) for medical diagnosis or treatment.
Image-based detection for COVID-19, early-stage lung cancer detection, a machine learning algorithm to find epigenetic markers for schizophrenia, algorithms to better understand the distribution of chronic pain – these are a just few stories that have arrived in my inbox.
I can almost feel the excitement of researchers as they imagine how AI-driven solutions based on their breakthrough research will be put into action to deliver better patient outcomes by healthcare providers around the world.
Without trying dampen these incredibly intelligent innovators’ enthusiasm, there are some barriers to the adoption and commercialisation of AI-powered solutions. Some of the biggest are to integrate them and exchange data securely with existing health technology systems, and ultimately to get them into the hands of clinicians who can trust and rely on them.
Interoperability – or exchanging data between applications and systems in a completely unambiguous way – is fundamental to digital healthcare technology. Whether it comes to caring for patients or analysing the evidence for new medical treatments, new solutions cannot exist in isolation.
The efficacy of AI-driven solutions must also be demonstrable to healthcare providers based on the data they hold about their patients, or that government agencies hold in relation to their populations. And to be useful, solutions must integrate with the systems and workflows that clinicians use every day.
Interoperability a major hurdle for AI solutions
AI may give a new healthcare solution cutting-edge capabilities, but it is unlikely to progress beyond a proof of concept unless it is built on a foundation of interoperability. To bring new AI-powered solution to market, solutions developers need to work with a range of healthcare data standards and the applications that use them.
The UK National Health Service (NHS), for example, has mandated the use of HL7® V2 and HL7 FHIR® to simplify and enable interoperability with new solutions and their governance. Healthcare solutions providers must support these standards if they want to be adopted by the NHS or interact with its existing systems. While not necessarily mandated, these and other data standards are also widely used by healthcare providers around the world, including those in the Asia Pacific region.
Companies developing AI solutions need to consider questions of scalability and interoperability early on in the development process. They should have a strategy for how their solutions fit into and interact with the data infrastructures of the healthcare providers they want to work with. And they should plan for success and consider how their solutions can be scaled quickly to meet the needs of a global market.
Developers don’t know what they don’t know
Despite their ability to innovate, however, solutions developers don’t always know what they don’t know. Many lack an understanding of interoperability requirements, or lack the skills or technology solutions to implement them. Start-up companies in particular should be aware that they cannot easily anticipate what data infrastructures they will be required to align with, or how quickly the volume and velocity of data they will have to handle will grow.
The easiest way to align with the different data infrastructures employed by healthcare providers in different markets is to implement a healthcare data platform strategy. This should allow developers to utilise comprehensive healthcare interoperability capabilities with their solutions as required and scale up to meet the demands placed upon them.
We are working with one company, Cognetivity, that has embraced a data platform approach. Cognetivity has a developed an AI-powered test to detect dementia years before it would otherwise become noticeable. The test leverages the ‘food or fear’ response which human beings have developed about animals. Patients are shown images of animals and an AI engine measures the accuracy and speed of responses and analyses the data to assess the patient’s risk of Alzheimer’s.
Because its solution is based on a data platform, Cognetivity has been able to rapidly integrate with existing healthcare systems at the NHS in the UK. In the early stages of adoption, this has allowed it to analyse existing demographic data to identify which patient cohorts would benefit most from being tested. It also expects to integrate with existing patient histories to perform more detailed analysis in the future.
Benefits of a data platform approach
Within a short space of time, Cognetivity has been able to work with ten NHS trusts on research projects and implement commercial solutions at two of them. Given that Alzheimer’s affects more than 50 million people worldwide, the potential need to scale the solution is enormous. Within the United States alone, the US Alzheimer’s Association estimates that more than $7 trillion could be saved through earlier clinical interventions.
In Australia, New Zealand, and increasingly across Asia Pacific, we are starting to see healthcare providers implementing their own data platforms to take advantage of the next wave of AI-powered solutions.
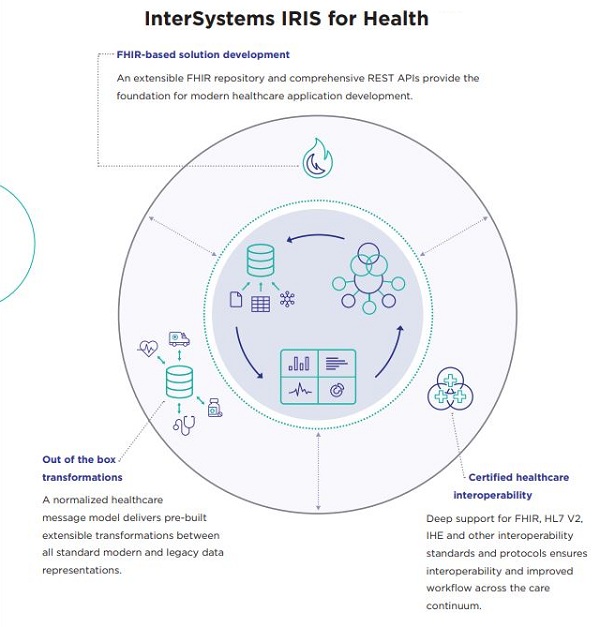
One of our customers, a group of hospitals and clinics in regional Australia, is using InterSystems IRIS for Health™ to make all healthcare data within their different facilities available for artificial intelligence & machine learning (AI/ML), business intelligence (BI) and clinical intelligence in real time. By embracing digital innovation, the organisations plan to improve clinical outcomes and patient experience, and optimise the use of resources.
While this makes it much easier to adopt innovative new solutions, developers cannot assume that providers will have their own healthcare data platform. Regardless of how innovative or beneficial new AI-driven solutions are, if healthcare providers have to do the heavy lifting of data integration, adoption will be limited.
And that would mean some very disappointed AI mavericks, not to mention poorer clinical outcomes for millions of patients who could miss out on the application of their breakthrough research.




















