Respiratory viruses – including SARS-CoV-2, influenza A and B, and RSV – pose a major public health threat every year. The seasonal nature of these viruses leads to sudden surges in cases during winter, putting strain on healthcare systems. However, there is still a degree of unpredictability over when they will emerge, and which strains will dominate, making it incredibly challenging for healthcare providers to prepare for upcoming seasons. There are also several factors that can determine the timing and severity of flu seasons, such as sudden influxes of tourists in popular winter destinations, or viral mutations that affect diagnostic testing. To manage these unpredictable outbreaks, hospitals must ensure they are well-prepared for the upcoming winter season with accurate and timely diagnostic testing.
Variations in viral rates and timings in Nordic countries
Management of the winter respiratory virus season is always challenging, as the timeline of peaks for each virus varies every year, and even between countries. For example, the 2022/23 influenza season in Norway and Denmark was prolonged, marked by an early, sharp peak around Christmas, followed by two smaller peaks taking the season right up to April.1,2 In contrast, the 2023/24 Norwegian flu season developed more gradually, with influenza activity peaking at a lower intensity.1 The 2023/24 season in Denmark peaked at week 51, when 1,870 people were diagnosed, leading experts to expect an early season.3 However, this dropped off dramatically over Christmas, resulting in an unexpected second peak in January.3
For SARS-CoV-2, the Nordic regions had a relatively low number of cases during the pandemic and the following years compared to other European countries, however there was great disparity between the countries in timings and excess mortality.4 Sweden experienced high excess mortality in 2020, and lower in 2021, whereas Denmark, Finland and Norway experienced the opposite, with excess mortality peaking in 2022.4 This may partly be explained by the early roll out of the COVID-19 vaccine in Sweden.4
The demand on healthcare services each winter is further complicated by rates of RSV increasing across most of Europe, including the Nordic region.5 It is estimated that 28 to 60 percent of respiratory tract infection hospitalisations of children under three months are associated with RSV in Denmark, Norway and Sweden,6 and all three countries have reported three or more consecutive weeks of RSV positivity above three percent since 2022.5
Emerging viral threats
The predominant strains of each virus vary year-to-year, but they can also fluctuate within a single season; the first peak in the 2022/23 influenza season in Norway was dominated by A(H1N1) strains, while the second featured significant levels of both A(H3N2) and B/Victoria viruses, and the final was dominated by B/Victoria-lineage viruses.1 Understanding the prevalence of influenza strains is critical as, occasionally, strains appear that create a major public health emergency. For example, particularly virulent strains of influenza A(H1N1) were responsible for the 1918 and 2009 pandemics, with the former resulting in an estimated 50 million deaths worldwide.7 The constant evolution of new influenza strains in birds has forced the European Centre for Disease Prevention and Control to encourage enhanced influenza surveillance during the coming 2024 winter season, with guidance on influenza A and B testing for all patients admitted due to respiratory or other influenza related symptoms.8 As a result, the Public Health Agency of Sweden has tightened surveillance of influenza.9
The hidden threat of new strains
PCR testing offers greater specificity and sensitivity compared to immunoassay or culture-based methods,10 positioning the technology as the most effective method for monitoring respiratory viruses. However, the rapid evolution of novel viral strains, driven by their ability to cross between a wide range of hosts,8 also threatens the effectiveness of even these molecular tests, as these viruses can mutate to evade detection. A 2022 study found notable issues in the detection of A(H3N2) during the 2021-2022 influenza season in Denmark.10 Mutations in the primer binding sites of the matrix gene in A(H3N2) enabled it to evade detection by several commercially available diagnostic platforms, resulting in high rates of false negatives, particularly from assays that rely solely on the matrix gene for detection.11
Misdiagnosis from inadequate testing methods could have serious repercussions by compromising infection control measures, potentially leading to improper isolation and treatment, which increases the risk of hospital-acquired infections spreading among patients and staff. This emphasises the need for continuous surveillance of circulating influenza strains and adjustments to diagnostic assays to maintain their sensitivity. By opting for a test that can detect multiple targets, healthcare providers can reduce the risk of viruses evading detection, helping to ensure that patients get an accurate diagnosis.11
A more efficient approach to testing
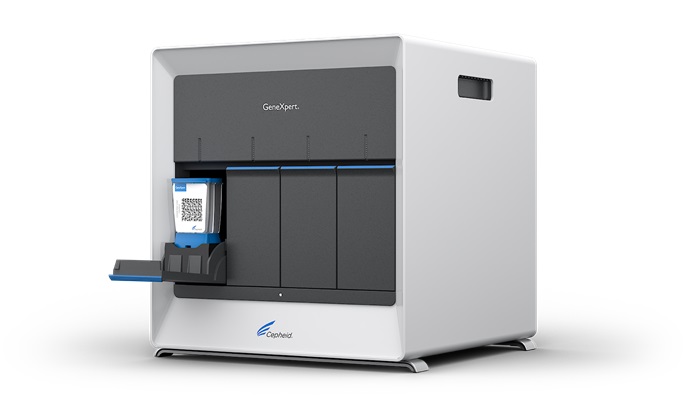
The seasonal surge in respiratory virus tests during winter adds to the strain on labs already burdened with high testing volumes for various conditions. To address these challenges, many hospitals have turned to point-of-care (POC) PCR testing for respiratory viruses, aiming to speed up time-to-results and reduce the pressure on central laboratories. This can help to deliver accurate and actionable results with large reductions in result turnaround time compared with centralised laboratory PCR testing.12 Multiplex PCR assays – such as the Xpert® Xpress CoV-2/Flu/RSV plus from Cepheid – take this one step further, streamlining the diagnostic process by allowing the detection of multiple pathogens from a single sample, eliminating the need for several swabs. In POC settings, multiplex PCR tests for SARS-CoV-2, influenza A and B, and RSV have demonstrated high sensitivity and accuracy, performing on par with individual tests for each virus, but with the added advantage of simultaneous detection.13 The faster turnaround times provided by these tests can help to triage high risk patients that need to be treated with antiviral drugs, ultimately reducing the length of hospital stays and decreasing costs.14 Crucially, these tests target unique sequences in three SARS-CoV-2, three influenza A, two influenza B, and two RSV genes, reducing the chances of new variants evading detection. By encompassing a wide range of genetic variations without sacrificing accuracy, the test helps to reduce false negatives and ensure effective surveillance as these viruses continue to evolve.11

Summary
The outlook for the upcoming winter remains uncertain, but data from the southern hemisphere indicates a rise in cases of both influenza and SARS-CoV-2.15 As healthcare settings brace for the pressures of winter, investing in POC PCR testing early, before the season hits, enables providers to respond quickly to respiratory threats and mitigate the impact of sudden surges in cases. However, as viruses continue to evolve and new influenza strains emerge, it is important to select tests that amplify several targets for each pathogen to avoid novel strains evading detection. By doing so, healthcare providers can be better prepared to manage increased patient loads and protect public health as winter approaches.
References
- Norwegian Institute of Public Health (2024). Interim influenza Virological and Epidemiological season report prepared for the WHO Consultation on the Composition of Influenza Virus Vaccines for the Northern Hemisphere 2024/2025. https://www.fhi.no/contentassets/de9d225ea2994b328b55e175f0688ba1/niph_nic-norway-interim-2023-2024-influenza-season-report-for-who-vcm-february2024.pdf
- Statens Serum Institut. (2023). Influenza 2022/2023. https://en.ssi.dk/surveillance-and-preparedness/surveillance-in-denmark/annual-reports-on-disease-incidence/influenza-2022-2023
- Statens Serum Institut. (2024). Integrated surveillance of respiratory infections in 2023/24 – combined report. https://en.ssi.dk/surveillance-and-preparedness/surveillance-in-denmark/annual-reports-on-disease-incidence/integrated-surveillance–of-respiratory-infections-in-2023-24—combined-report
- Forthun, I., et al. (2024). Excess mortality in Denmark, Finland, Norway and Sweden during the COVID-19 pandemic 2020–2022. European Journal of Public Health, ckae091.
- European Centre for Disease Prevention and Control. (2022). https://www.ecdc.europa.eu/sites/default/files/documents/RRA-20221128-473.pdf
- Del Riccio, M., et al. (2023). Burden of respiratory syncytial virus in the European Union: estimation of RSV-associated hospitalizations in children under 5 years. The Journal of infectious diseases, 228(11), 1528-1538.
- St John A, Price CP. (2014) Existing and Emerging Technologies for Point-of-Care Testing. Clinical Biochemistry Review. 35(3), 155-67. PMID: 25336761; PMCID: PMC4204237
- European Centre for Disease Prevention and Control. (2024). Enhanced influenza surveillance to detect avian influenza virus infections in the EU/EEA during the inter-seasonal period. https://www.ecdc.europa.eu/en/publications-data/enhanced-influenza-surveillance-detect-avian-influenza-virus-infections-eueea
- (2023). Surveillance of communicable diseases. https://www.folkhalsomyndigheten.se/the-public-health-agency-of-sweden/communicable-disease-control/surveillance-of-communicable-diseases/
- S. Centers for Disease Care and Prevention. (2024). https://www.cdc.gov/mmwr/volumes/73/wr/mm7316a2.htm
- Jørgensen, R. L., et al. (2022). Emergence of circulating influenza A H3N2 viruses with genetic drift in the matrix gene: be alert of false‐negative test results. Apmis, 130(10), 612-617.
- Brendish N, J., et al. (2020) Clinical impact of molecular point-of-care testing for suspected COVID-19 in hospital (COV-19POC): a prospective, interventional, non-randomised, controlled study. Lancet Respir Med. 8(12), 1192-1200.
- Leung E, C., et al. (2021). Evaluation of the Xpert Xpress SARS-CoV-2/Flu/RSV Assay for Simultaneous Detection of SARS-CoV-2, Influenza A and B Viruses, and Respiratory Syncytial Virus in Nasopharyngeal Specimens. Journal of Clinical Microbiology. 59(10). 1128/jcm.02965-20. https://doi.org/10.1128/jcm.02965-20
- Vecino-Ortiz, AI., et al. (2018). Impact of a multiplex PCR point-of-care test for influenza A/B and respiratory syncytial virus on an acute pediatric hospital ward. Diagnostic Microbiology and Infectious Disease. 91(4). 331-335.
- World Health Organization. (2024). Global respiratory virus activity weekly update No. 489. Accessed 22nd August 2024.