Despite facing perhaps the greatest challenge seen in a lifetime, the COVID-19 pandemic highlighted what makes the healthcare industry such a resilient field. When thinking about the past three years, words like adaptability, collaboration and innovation come to mind.
One example is how hospitals modified previously established protocols during COVID-19 to provide resource-intensive care to patients, while also continuing routine hospital care. With each major COVID-19 outbreak, frontline healthcare providers were deployed to areas outside their clinical area of expertise to address an increased number of admitted patients.1 While this exhibited hospitals’ ability to evolve during a crisis, it also amplified the need to rethink daily protocols and incorporate multidisciplinary care models and dedicated care units to more efficiently care for patients.
This is something TriVent Healthcare incorporated long before the pandemic.
Taking A Multidisciplinary Approach
As many have come to realize, prolonged dependence on mechanical ventilation is an emerging public health problem, especially after a critical illness. Nearly 40% of patients entering the intensive care unit (ICU) require mechanical ventilation and nearly 20% of these patients are expected to have increased ICU stays due to difficulty weaning.2
It’s become vital to incorporate a multidisciplinary approach for patients receiving prolonged mechanical ventilation (PMV). Patients receiving PMV generally exceed the median length of stay in a hospital and have a disproportionate readmission rate as compared to those ICU patients who do not require PMV.3 Typically, these patients are treated by a dedicated team within the ICU led by a pulmonologist who is responsible for making decisions and writing orders.
While a focus on the lungs is important when treating ventilated patients, moving to a multidisciplinary approach with respiratory therapists leading patient treatment, along with a dedicated team of physical therapists, occupational therapists, speech pathologists, acute care trained nurses and dedicated case managers is suggested for future care models. This allows for more time with the patient, which enables early mobility and enhanced rehabilitation opportunities.
Studies show that a dedicated, multidisciplinary weaning unit for PMV patients not only reduces overall length of stay, but also shows an improvement in patient survival, functional status, reduction in ventilator days or mechanical ventilation at discharge, and quality of life.3 This clearly illustrates an increased need for dedicated ventilator care units within hospitals.
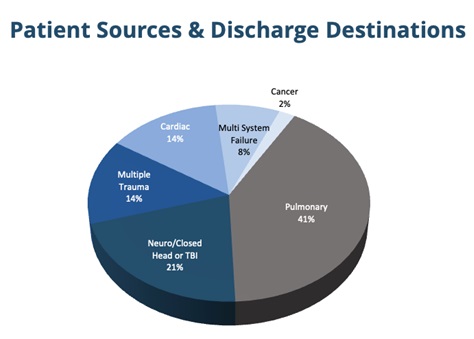
There are numerous reasons why patients are placed on ventilator care. Often, respiratory failure is secondary to the trauma that requires the use PMV. That’s why it’s important to have a dedicated team who know how to properly care for patients with varying primary health issues including trauma, stroke and congenital heart failure.
Dedicated Ventilator Rehabilitation Units
In addition to a multidisciplinary team, PMV patients benefit from hospitals establishing one central location for care.
For example, TriVent Healthcare partnered with the University of Alabama at Birmingham Hospital (UAB Hospital) in October 2016 to open a Special Care Unit dedicated to improving the care for patients experiencing PMV for more than 21 days. The goal was to reduce ventilator days, improve patient quality and reduce the overall length of stay. The Special Care Unit is consolidated into a designated section of the hospital, which provides an optimal care flow, and all patients in the unit receive individualized daily, multidisciplinary care. This allows for more patient interactions with a higher patient-to-clinician ratio, which results in more opportunities for early rehabilitation.
From October 2016 to July 2022, patients discharged from the Special Care Unit at UAB Hospital showed an achieved ventilator liberation rate of 85.4%, nearly 40% higher than the national average. What’s more, the success rate of weaning patients from the ventilator in a typical ICU is only between 30% and 53%.4 Moving these patients from the ICU to a dedicated ventilator care unit enhances liberation success as patients receive individualized care from a multidisciplinary team.
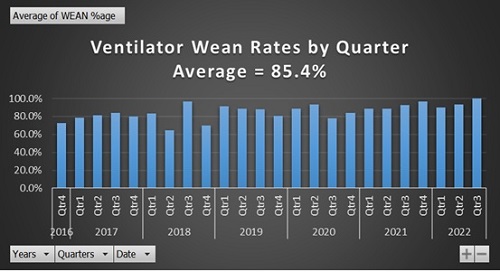
This confirms previous studies and strongly suggests the correlation between successful liberation in PMV patients.
Updating Industry Terminology for Care Clarity
While some hospitals report high wean rates like those achieved by TriVent Healthcare, it’s important to have updated protocols to address the difference between “wean rates” and “liberation rates.”
Many hospitals define wean rate as the process of removing all admitted patients from ventilator care – including post-operative and short-term trauma patients who may not have been intubated, but not received a tracheostomy. Dedicated ventilator liberation units like TriVent Healthcare prefer the term liberation rate as opposed to wean rate as they are referring to complex PMV patients who received a tracheostomy and have since been successfully removed from ventilator care altogether. It’s important for hospitals to make this distinction between wean rate and liberation rate when reporting ventilator liberation rates, as short-term ventilated patients and PMV patients are cared for differently.
More and more, hospitals are incorporating dedicated ventilator units with multidisciplinary teams like TriVent Healthcare into their facilities. This type of care model improves the care flow within the hospital and helps reduce the length of stay of the patient – ultimately resulting in shorter recovery times and lowering the chances for readmission.
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7918807/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7483008/#:~:text=The%20success%20rate%20of%20weaning,failure%20%5B3%2D5%5D
- https://pubmed.ncbi.nlm.nih.gov/12602416/
- https://journals.lww.com/ccmjournal/Abstract/2008/03000/Prolonged_acute_mechanical_ventilation,_hospital.9.aspx




















