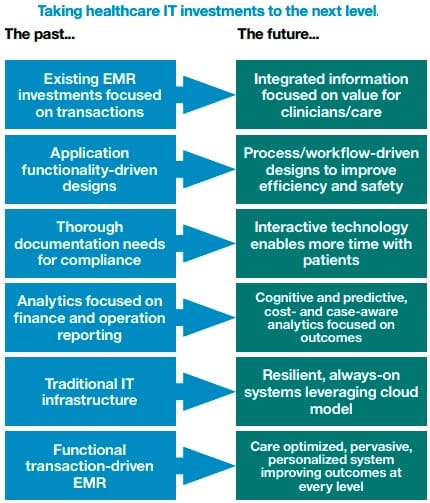
Over the past 30 years, hospitals and health systems have made sizeable investments in the deployment of electronic medical records (EMR) systems. Driven by revenue capture, compliance demands and transactional interdepartmental communications, earlier implementations largely preserved existing operational processes, while more recent deployments have focused on the clinical process implications.
The desire to demonstrate meaningful use has heightened adoption and clinical utilization; however, opportunities for further optimization across disparate hospital systems and processes still remain. Today, healthcare enterprises seek new ways to realize value beyond their EMR investments by identifying strategic IT initiatives that will contribute to measurable business objectives and care outcomes.
Seamless integration of highly diverse technologies can facilitate faster and safer throughput of patients, create more capacity through efficiencies and help contain costs for healthcare organizations. It’s not just about the EMR anymore. It’s about integrating and liberating data from all sources to deliver information in a format that is both consumable and convenient for the user.
To obtain a true return on investment—before, during and after an EMR is deployed organizations are adopting both technology and process improvement strategies with a patient-centric focus to facilitate exchange and analysis of relevant information, ensure privacy and security, and create greater efficiencies in both business and clinical processes. 1
The next phase for IT
As transformation of the industry accelerates, healthcare organizations are rethinking business models, partnerships and delivery of services. The boundaries between payers and providers are blurring, new payment models are emerging and the elements of risk are shifting. And perhaps most significant, there is an increasing shift away from the volume-based, fee-for-service model that has dominated the industry for decades toward a more performance-based, outcomes-driven approach.2 As analysts predict the “industrialization of healthcare” continues, provider organizations will need to serve more patients and deliver better quality care with a higher degree of standardization and productivity across organizations and individual providers. 3
Cost containment initiatives, process efficiency, IT optimization and business analytics can all contribute to greater operational effectiveness. Healthcare enterprises need to make hard, thoughtful and informed decisions about every aspect of their operations. With multi-million dollar investments in EMR technologies and growing achievement in meaningful use initiatives, the focus is now turning to the next level of return.
Technology plays a critical role in enabling healthcare transformation. Technology can improve operations, support collaboration and provide the groundwork for data-driven decision making. The ability to capture, integrate and analyze data across different stakeholders, care settings and geographies is essential, as is modernizing infrastructure to increase agility. New modalities, diagnostics and innovative medical devices, as well as the use of telemedicine and remote monitoring, add to technological enablement by increasing access and expertise.
A key enabler of transformation, technology eliminates current borders of the business by overcoming barriers such as distance, knowledge or practice. Today’s healthcare industry can now take advantage of information technology as so many other industries have—to innovate business models and eliminate disparities in access to care.
Working with clients and partners around the world, we see the focus of IT moving to the next level of return as stakeholders seek demonstrated benefits. Today, healthcare organizations are focused on leveraging IT solutions to improve insight, optimization, engagement and organizational agility:
- Insight:Â Access and analyze data to create insights and standardize processes to better measure, understand and improve health outcomes.
- Optimization:Â Optimize workflows and systems to improve operational efficiency, safety and compliance.
- Engagement:Â Increase engagement levels of individuals and across the enterprise through enhanced access, collaboration and learning.
- Agility:Â Build infrastructures that provide scale, resiliency and continuity to support operations and new services ensuring security, privacy and compliance.
Insight
As the new natural resource of the digital age, data can provide insights to improve quality and outcomes, lower costs and increase value for the industry. When captured and managed effectively, it becomes the fuel for competitive advantage. Indeed, big data and analytics are transforming healthcare. Organizations are growing their analytics capabilities and skill sets to gain insights that improve operations. They are also turning to new types of data, such as unstructured and streaming data, and making strides toward smarter care and improved health outcomes.
Improving operations
Big data and analytics enable an organization to gain deeper insights into its clinical and organizational operations—and these insights can help improve patient flow, safety, quality of care and the overall patient experience. Such was the case with South Tyneside NHS Foundation Trust, a provider of acute and community health services in northeast England that needed a better understanding of how its hospitals operated to improve resource allocation and wait times.4
 South Tyneside implemented an analytics solution that not only automates the reporting of performance metrics, but also supports strategic planning and day-to-day operations. With the solution, South Tyneside has been able to build compelling business cases for investment in new services based on data from thousands of patient visits and provide accurate insight to support operational decision making, such as predicting future vacancies and occupancy rates.
South Tyneside implemented an analytics solution that not only automates the reporting of performance metrics, but also supports strategic planning and day-to-day operations. With the solution, South Tyneside has been able to build compelling business cases for investment in new services based on data from thousands of patient visits and provide accurate insight to support operational decision making, such as predicting future vacancies and occupancy rates.
Using these analytics has made it easier to manage emergency admissions, schedule procedures and plan for human resources requirements, including how many nurses are required to support the patient load. The solution enabled the creation of a wide range of reports, dashboards and scorecards that provide users at all levels of the organization insight into day-to-day operations, all of which has helped improve service levels.5
Leveraging unstructured and streaming data
In addition to the structured data typically found in an EMR, unstructured data remains an untapped resource for many organizations. In fact, it’s estimated that close to 80 percent of all healthcare data is unstructured, in the form of clinical notes, test results and images, discharge summaries, patient communications, videos, etc.6 However, healthcare’s traditional data management approaches do not take advantage of the insights available through the mining of this unstructured data.
To better support decision making, organizations need solutions that extract insights from all types of data. UNC Health Care (UNCHC), a not-for-profit integrated healthcare system in North Carolina, understands this. Using a big data and analytics solution, UNCHC implemented a system that allows clinicians to quickly access and analyze unstructured patient data using natural-language processing.
With the ability to see and interpret both structured and unstructured data, UNCHC has accessed and analyzed huge quantities of unstructured content contained in patient medical records, including the detailed narratives authored by physicians and other caregivers. This data was evaluated to provide context for identifying at-risk individuals for timely intervention and targeted treatment plans. UNCHC demonstrated how the system can be used to extract predictors of readmission risk from text-based clinical notes to help provide safer care for high-risk patients and reduce re-admissions.7

Analytics solutions can also reveal insights from streaming data. New technologies to analyze streaming data from medical devices and wearable sensors are opening up new worlds of medical discovery and intervention, as well as employing expanded analytics capabilities that include predictive and cognitive capabilities.
For example, a leading U.S. university and research medical center has launched a pioneering project to create advanced, predictive medical care for critical patients through real-time streaming analytics of physiological data from critical care monitors. With the ability to analyze more than 100,000 real-time data points per patient per second, the researchers are working to identify patterns that could indicate serious complications like sepsis, heart failure or pneumonia. The overall goal is to provide real-time medical insights to clinicians.
Taking a smarter care approach
The deep insights gleaned through big data and analytics are key to smarter healthcare. By leveraging new and existing data sources and analytic innovations, healthcare providers not only can deepen their understanding of individuals’ needs, but also facilitate cross-agency collaboration, case management, and program access and delivery. In addition, they can uncover valuable insights into lifestyle choices, social determinants and clinical factors.
Context-based insights from social and clinical analysis allow care professionals to segment populations by risk profiles, inform care approaches for individuals, and proactively manage finite care resources faster and more efficiently, leading to improved outcomes.
Consider, for example, a European public health services provider that has taken a smarter care approach. The provider, which has a large chronic disease burden, launched a new care coordination program that delivers an integrated view of patient data to support primary, hospital and social care.
Physicians, nurses and social workers now have a 360-degree view of each patient and create care plans tailored to each individual’s needs. The program has reaped benefits for the provider and its patients, including reductions in emergency room visits, hospital readmissions and program costs; the ability to assemble assessments and care plans in hours rather than months; and improved collaboration across the community of care.
Optimization
Health systems are under heavy pressure to contain cost without compromising quality of care. The good news is there are enormous opportunities for cost containment through process improvements and increased workflow efficiencies, particularly in streamlining steps that do not contribute directly to patient care or outcomes. Investing in business process management, automation of asset management, and equipment maintenance management can help positively impact the bottom line.

Business process management
While many traditional EMR implementation projects offer improvements in terms of transactional clinical processes, they often do not solve the larger-scale operational process problems. Hence, hospitals are beginning to focus on process design and improvement as a discipline to provide more patient-centered and harmonized care. Implementing business process management solutions “on top” of existing EMR systems can avoid the costly—and often painful—process of changing or re-implementing the EMR system.
The Ottawa Hospital leveraged business process management and mobile technologies to create a comprehensive care process management platform with the goal of improving patient flow and communications across the care team. The goal was to relieve clinician time by using electronic closed-loop consults and providing easy access to patient information from the EMR to create a “circle of care” focused on the patient.
The care management platform allows a view of a patient’s most current projected discharge date based on the care team’s latest input, with required specialists and clinicians automatically notified when a patient’s status changes. The enhanced communication and coordination between team members not only help improve patient flow through the emergency department, but also contribute to the overall patient experience.8
Facility and asset management
Hospitals, clinics and other large healthcare providers consist of complex systems upon systems, with both personnel- and asset-intensive operations. In large, complex environments such as these, assets can be difficult to find and sometimes get lost or stolen. Subsequently, additional, spare and replacement assets are purchased, while existing assets are not fully utilized. Innovative hospitals are addressing the problem with real-time location approaches, such as radio frequency identification (RFID), ultrasound technology or indoor proximity systems.
For example, a U.S. hospital implemented real-time tracking of medical equipment to ensure that life-saving medical devices are instantly available and expertly maintained. The hospital’s solution uses sensor technology to automatically track equipment, alert staff when the required level of equipment is running low and help ensure compliance with patient safety regulations.
What we are doing is putting process orchestration and process models in place, so that you can literally see the characteristics of the hospital system. You can see, for example, that the flow in the emergency department is too fast to be taken up in the admitting units, and you can then influence that. Wayne Gretzky
As another example, consider how a major teaching hospital in the United States sought to “do more with less” by utilizing an integrated asset and service management system to provide visibility across departments and sites. The organization began proactively managing assets to ensure their availability and peak performance through the entire lifecycle, thereby lowering capital and operational expenditures associated with these increasingly complex assets.
In addition to necessary maintenance, healthcare facilities must ensure they meet various regulatory requirements related to operations and devices. Breakdowns or ill-timed maintenance can be wasteful, destructive and inefficient. Not unlike other industries, downtime of key machines—in healthcare, key diagnostic machines—translates to lost revenue; hence, there is a focus on optimizing physical assets and operational processes to ensure they are functioning as intended and the return on investment (ROI) optimized.
State-of-the-art asset management is required, along with innovative approaches such as predictive maintenance, which allows technical staff to prevent equipment malfunction rather than simply react to failures. A U.S. healthcare provider had the foresight to extend a design/construction tool used in building a new hospital to manage the hospital’s assets after construction. By integrating the hospital’s asset management software and its design/construction tool, the provider not only saved approximately 600 hours of manual data entry time and precious square feet of document storage space in the new building, it will potentially save US $225,000 a year. Equally important, the staff can view the specs and maintenance histories of more than 5,000 assets with unprecedented efficiency.
Engagement
One of the most transformational drivers in healthcare, mobility represents a new opportunity for personal engagement and enterprise efficiency. Indeed, today’s mobile and social technologies are helping hospitals redefine patient-provider relationships, as well as enhance interactions and communication among and within their teams.
For example, a Canadian healthcare facility increased both communication and safety through a wireless communication device. Previously, staff communicated via overhead pages and phone calls routed through an outside switchboard, which frequently resulted in extended wait times. Now, with one tap on a wireless communication badge, a staff member can open a connection with other employees and, with two taps, report a “code white”—a violent incident—alerting the hospital’s entire security force. With the program, the hospital’s response rate to code whites decreased from an average of two-and-a-half minutes to 59 seconds. The solution has also simplified collaboration among staff members with instant two-way communication, helping improve the quality of patient care.
 Mobile solutions are also opening new avenues for engagement and extension of services across care communities. Collaborative technology can enhance communication in hospitals, primary care facilities and at home, while social media and mobile technology provide multiple communication channels for patients and family to stay in touch with care providers and other patients. In complex medical situations such as chronic diseases, patient and family member empowerment is particularly important.
Mobile solutions are also opening new avenues for engagement and extension of services across care communities. Collaborative technology can enhance communication in hospitals, primary care facilities and at home, while social media and mobile technology provide multiple communication channels for patients and family to stay in touch with care providers and other patients. In complex medical situations such as chronic diseases, patient and family member empowerment is particularly important.
Children’s Medical Center of Dallas launched an online environment to involve both children and their families in the process of care. The social network lets both past and present patients and their families share stories and support. The network is divided into communities based on various specialties, including gastroenterology, neurology and cardiology. As for the children, they enjoy the chance to socialize with other patients with similar conditions to exchange information and share experiences.9
New mobile technologies and mobile health, or mHealth, initiatives are extending the industry’s reach and capacity to provide health services in remote and underserved areas. And as social and mobile networks have empowered individuals, healthcare organizations are in turn providing multi-channel approaches, varied settings and convenient locations to define new relationships, as well as coordinate and improve efficiency of service. Connectivity—across device and technology—is also enabling the industry to engage individuals in their own health and wellness in unprecedented ways.
Consider the European health organization that developed a best practices program with telemedicine and tele-monitoring to support its type 2 diabetes patients’ compliance with diet, exercise and medication regimens. Rather than requiring patients to visit their doctors’ offices for more routine checkups, this in-home diabetes monitoring program uses telemedicine to allow physicians to closely follow patients’ at-home compliance.
Medical devices, such as blood pressure and blood glucose monitors and scales, are linked to a cell phone, which automatically sends the patient’s data to a “diabetes diary” database. There, an algorithm compares expected results with actual values and sends an immediate notification to the physician if the value exceeds a critical limit. This allows the physician to react quickly to modify the patient’s treatment, helping improve patient treatment and avoid the many complications that accompany this disease.
New social technologies are also expanding caregivers’ base of knowledge by facilitating increased consultation and information sharing among health professionals around the globe. For example, Boston Children’s OPENPediatrics platform provides training for medical professionals using a unique on-demand, interactive, digital and social learning experience, equipping them to perform life-saving procedures and treatments for children who would not otherwise have access to intensive care. The cloud-based education and collaboration platform brings together a global community of healthcare workers, students and medical experts in a continuous learning environment and delivers curated, expert knowledge in the form of training videos, sophisticated medical simulations, lectures and best practices. Caregivers not only learn from experts how to diagnose and treat acute childhood illnesses, they also can interact with each other, sustaining ongoing discussions about effective practices in a clinical setting and growing a rich repository of combined knowledge in the process.10
 Agile foundations
Agile foundations
To compete in today’s fast changing healthcare environment, healthcare organizations need to ensure their IT investments provide both the agility and scalability necessary to meet the demands for new services, partnerships, opportunities and threats. Yet, many healthcare IT environments currently address administrative needs (such as health plan enrollment, physician or hospital billing and claims processing) better than they do their lines of business needs.
Today’s healthcare IT environment must be capable of capturing, storing, analyzing and appropriately sharing information about individual patients and patient populations without unplanned downtimes. It also must be capable of rapidly generating and managing new clinical knowledge and easily incorporating it into clinical processes and workflows for decision making related to health promotion and care delivery. This environment also must facilitate appropriate interactions among constituents. And it must do all this in a secure manner.
Security, privacy
Healthcare organizations store, maintain and transmit huge amounts of data to support the delivery of efficient and proper care. While data privacy is critical, the security issues facing healthcare organizations clearly extend across a much broader set of concerns—and encompass much more than achieving compliance. Complicating matters, the healthcare industry continues to be one of the most susceptible to publicly disclosed data breaches.11
Take a holistic approach to security
- Understand where the data exists: To protect sensitive data, you must know where it resides and how it’s related across the enterprise.
- Safeguard sensitive data, both structured and unstructured: Structured data contained in databases must be protected from unauthorized access. Unstructured data in documents and forms requires privacy policies for redaction and enforcement.
- Protecting non-production environments: Data in non-production, training and quality assurance environments needs to be protected yet still usable during the application development, testing and training processes.
- Secure and continuously monitor access to data: Enterprise databases and file shares require real-time insight to protect and audit data access. Policy-based controls are required to rapidly detect unauthorized or suspicious activity and alert key personnel.
- Demonstrate compliance: Develop a holistic approach that can demonstrate compliance and provide proof to third-party auditors.
Today, too many hospitals and other healthcare facilities rely on outdated approaches implemented on aging infrastructures. At the same time, patients, families, visiting physicians, contract caregivers, insurance companies and government regulators require the exchange of and access to data—each with its own level of authorization. New insurance exchanges, both private and public, increase the amount of data shared throughout the healthcare supply chain, creating new challenges and new security requirements. In addition, medical devices such as heart monitors or lab equipment collect and store sensitive personal information.
Healthcare organizations need broader views of their environments and more comprehensive privacy and security control of their data than is typically afforded by specialized point products. Streamlined and simplified management —with built-in automation and ease of useis required to support security across the increasingly complex and rapidly changing environments. Healthcare organizations must take a holistic approach to protecting and securing their information.
Infirmary Health System in Alabama sought to automate and strengthen security and endpoint management to better protect data and meet HIPAA and meaningful use requirements. The organization, which includes hospitals, outpatient facilities and medical clinics, deployed a comprehensive security solution that helps staff secure endpoints and better detect and respond to threats across the organization. The solution analyzes event data from thousands of network and security devices, services and operating systems, and applications to help staff quickly see developing threats. With this comprehensive visibility, Infirmary can now detect and identify near-real-time offenses and threats. And with a unified security platform in place, it has met data security requirements for meaningful use, qualified for meaningful use funds and reduced security incidents significantly.12
Leveraging cloud
In the changing healthcare environment, cloud computing can be an enabler of organizational transformation. Leveraging the power of cloud, healthcare organizations can create dynamic infrastructures that can help improve operational speed and dexterity by optimizing and accelerating IT resources and service delivery. Cloud can also improve the economics of IT by optimizing availability and reducing complexity.
A number of forward-looking healthcare organizations are relying on cloud solutions to help lower costs, enhance the productivity of their infrastructure investments, and enable innovative ways to deliver service to consumers through social, mobile and analytics. For example, healthcare organizations are experimenting with cloud infrastructure services to reduce the cost of data center operations, while researchers are tapping into high-performance computing and file sharing.
Gaining experience with private clouds, organizations are acquiring greater visibility into the technologies, processes, staffing and costs that support their secure operations and are opening opportunities for public/private/hybrid clouds in the industry.
Medical grade and optical networks
Data networks are the backbone of hospital operations in the digital age. New hospitals and those undergoing reconstruction need to carefully consider their needs to ensure the resulting medical grade network is capable of handling the various devices, applications, etc.—and that it can adapt to handle future advances. Innovative approaches such as passive optical networks (PON) can better accommodate the growing needs of users who require instant-on systems and devices, as well as provide the necessary scalability and security.
Resiliency, continuity
Virtually every aspect of any business is vulnerable to disruption. Some resiliency and continuity issues could take a business offline for days, but even minutes of downtime can prove costly, particularly in a healthcare setting.
Clinical systems are crucial to a healthcare organization’s operations and, therefore, must be available around-the-clock, 99.999 percent of the time. There is no room for downtime, as it impacts not only a clinician’s ability to effectively treat a patient, but also care provider productivity.
Hospitals and other medical facilities must have adequate continuity planning for their critical business functions and ensure their daily operations continue seamlessly under all circumstances. Despite years of industry underinvestment in this area, analysts project healthcare providers will begin more heavily investing in data recovery and business continuity tools. Healthcare organizations are turning to intelligent and cloud-based data backup solutions to protect both data and business continuity of mission critical systems. They expect these solutions not just to protect data, but to also play a key role in supporting insightful business decisions. Intelligent data backup solutions make it easier for an organization to quickly access the information it needs, even in the wake of a service disruption, system outage or disaster.
Conclusion
Deeper insights, optimized processes, and increased engagement and collaboration—all supported by a robust foundation that enables greater scale and agility—can create a system in which information is captured intelligently in real time, shared securely across the complete spectrum of practitioners and made available to stakeholders. In such an environment, critical information is gathered from various sources and locations and delivered where and when it is needed in a form that improves delivery of healthcare—for patients and caregivers. The EMR was just the beginning. Now it’s time to continue the journey.
The IBM Digital Hospital Framework
Whether planning the development of new acute care and ambulatory facilities or modernizing aging technology infrastructure of existing hospitals, healthcare executives and their boards must endorse the big picture, understanding how departments interact within an enterprise and how different facilities across diverse care settings must work in a coordinated health system. In addition, understanding the dependencies and relationships between various IT programs and initiatives can help healthcare decision makers cope with the complexity of the numerous solutions and choice available to them.
A framework representing the various categories and components of IT — networks, storage, EHRs, care orchestration systems, etc. — can help executives understand how the IT elements in the framework relate to their larger strategic objectives. IBM provides a comprehensive framework based on digital hospital design and implementation experience.
How IBM can help hospitals transform
Enabling processes with technology requires a deep understanding of how all the “moving parts” work together. IBM works with healthcare facilities around the world to leverage information technology to provide enhanced operational effectiveness, deliver collaborative care for prevention and wellness, and achieve better quality of care and improved outcomes. IBM provides process, technology, architecture, integration and program management services to new digital hospitals or hospitals looking to digitally transform their infrastructure.
Sources
- “The digital hospital evolution, Creating a framework for the healthcare system of the future.” IBM Global Business Services. April 2013.
- “Redefining value and success in healthcare, Charting the path to the future.” IBM Healthcare and Life Sciences. IBM Software Group. February 2012.
- Hanover, Judy. “U.S. Healthcare Provider Predictions for 2014: IT Priorities in the Post-EHR Era.” IDC website. January 28, 2014. https://idc-community.com/health/healthcare-transformation/us_healthcare_provider_predictions_for_2014_it_priorities_in_the_pos
- “South Tyneside NHS Foundation Trust, Harnessing analytics for strategic planning, operational decision making and end-to-end improvements in patient care.” IBM Smarter Planet brief. 2013. http://www-01.ibm.com/common/ssi/cgi-bin/ssialias?subtype=AB&infotype=PM&appname=SWGE_YT_YU_GBEN&htmlfid=YTC03623GBEN&attachment=YTC03623GBEN.PDF
- Ibid
- “Harness your data resources in healthcare.” IBM website. http://www-01.ibm.com/software/data/bigdata/industry-healthcare.html
- “UNC Health Care relies on analytics to better manage medical data and improve patient care.” IBM press release. October 11, 2013. http://www-03.ibm.com/press/us/en/pressrelease/42179.wss#_ftnref1
- The Ottawa Hospital Achieves Process Innovation with IBM Software.” April 29, 2012. https://www.youtube.com/watch?v=SNSQTJmGoE4; “The Ottawa Hospital improves patient care and safety.” IBM Case Study. April 2012. http://www-01.ibm.com/common/ssi/cgi-bin/ssialias?infotype=PM&subtype=AB&htmlfid=WSC14404USEN#loaded
- Cerrato, Paul. “Children’s Medical Center Dallas Gets Social.” InformationWeek. Government. September 9, 2012. http://www.informationweek.com/it-leadership/childrens-medical-center-dallas-getssocial/d/d-id/1106151?
- “OPENPediatrics.” Boston Children’s Hospital website, accessed September 16, 2014. http://www.childrenshospital.org/research-andinnovation/research-initiatives/openpediatrics; “About us.” OPENPediatrics website, accessed September 16, 2014. http://openpediatrics.org/about-us/about-us-2/
- Wike, Katie. “Data breaches expected to surge.” Health IT Outcomes. January 6, 2014. http://www.healthitoutcomes.com/doc/data-breachesexpected-to-surge-0001
- “Infirmary Health System, Gains meaningful use dollars with improved security and audit reporting.” IBM Software Group. http://www-01.ibm.com/common/ssi/cgi-bin/ssialias?subtype=AB&infotype=PM&appname=SWGE_WG_WG_USEN&htmlfid=
WGC12356USEN&attachment=WGC12356USEN.PDF