With more than 3 million cataract procedures each year and a success rate of 98% or higher1, cataract surgery in the U.S. has become a highly refined art. In a typical cataract procedure, the surgeon makes two small incisions in the cornea, breaks up the hardened, discolored natural lens of the eye and removes it using ultrasound energy, and then replaces the lens with an artificial intraocular lens (IOL).
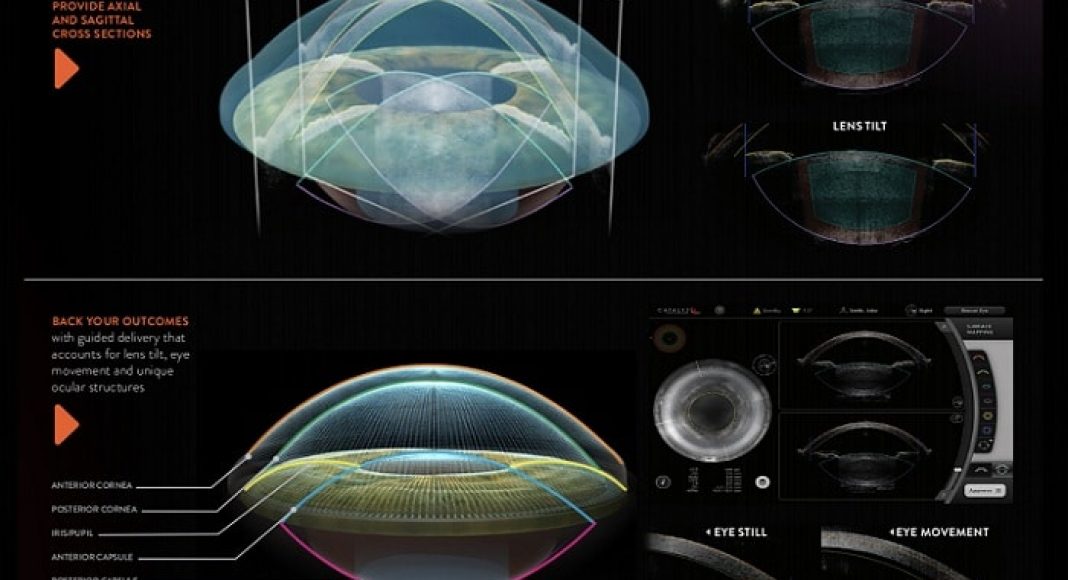
In recent years, femtosecond laser technology has been incorporated into cataract surgery, creating a more standardized, precise way of performing the complex tasks required for successful surgery. This has been made possible by the confluence of technological advances in imaging, lasers, robotics, and even artificial intelligence. For example, micron-level optical coherence tomography (OCT) technology allows the laser system to image the entire lens and anterior segment of the eye. Much like interventional radiologists depend on fluoroscopy to guide their procedures, we use OCT imaging to guide the femtosecond laser portion of the cataract procedure from start to finish.
The laser performs several parts of the cataract procedure. It can create the incisions through which the lens is extracted and the new IOL implanted; peripheral, arc-shaped incisions on the cornea to correct astigmatism; and a circular opening in the anterior lens capsule to give the surgeon access to the sclerotic nucleus within the capsule. For each of these steps, the laser replaces a blade or other manual tools. It can also pre-soften the lens, which is an entirely new function that can’t be done manually at all. Here, I’ll discuss the advantages of several of these steps,as I see them:
 Lens softening
Lens softening
Using laser energy to pre-soften the lens reduces the amount of ultrasound energy needed during the lens removal portion of the procedure. This may not make a huge difference in every case, but I certainly find it helpful in eyes with particularly dense cataracts. It also has some potential advantages in dealing with conditions such as Fuchs dystrophythat make the corneal endothelium more vulnerable to damage during surgery. Although this has not been proven, the laser can theoretically help prevent corneal edema and avoid the need for secondary surgical procedures in such cases.
Capsular opening
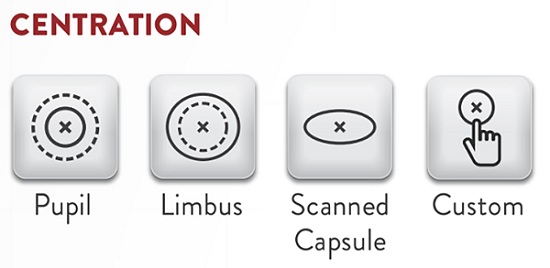
The Catalyslaser platform I use (Johnson &Johnson Vision) uses OCT imaging to scan the lens capsule and create a circular opening (the capsulotomy) exactly in the center of that capsule, where the IOL will fixate. For surgeons, the perfect circularity and repeatable size of these laser-created capsulotomies is impressive but it may be more just aesthetically pleasing. The size and shape of the opening helps to ensure a consistent overlap of the edge of the IOL to help stabilize it and prevent lens tilt, which can induce visual distortions. Having a perfectly centered capsulotomy also provides a mechanism for fixating a lens in the correct position in case of an intraoperative complication that results in the loss of posterior capsule support.
 Astigmatism correction
Astigmatism correction
Finally, the laser has become a very accurate tool for correcting lower levels of astigmatism and driving better refractive outcomes. In my practice it has contributed to an improvement in visual outcomes, with >80% of my patients functioning without glasses for distance, up from about 50% in 2016. Much of this is due to better control of astigmatism. More than 65% of patients presenting for cataract surgery have < 1.00 D of corneal astigmatism, which means they aren’t candidates for a toric IOL. 2However, someone with 0.50 or 0.75 D of astigmatism can still have rather poor vision, so I prefer to get every patient as close to zero astigmatism as possible. Femtosecond laser offers a precise correction at the time of surgery.
Better surgery even without the laser
I believe that using a femtosecond laser has also improved my manual surgery technique, especially when it comes to perfecting the capsular opening. The laser serves as a kind of robotic “master surgeon” for me to emulate. I’m continuously reminded of—and striving to replicate—the ideal capsulotomy size, shape, and centrality that the laser creates.
Additionally, because vertical chopping is regarded as the most appropriate technique to apply to a pre-softened lens, I’ve learned how to perform this efficient technique. Learning it on laser-softened lenses made this technique easier to master and apply to regular cases, as well. I now use a vertical chop technique in all of my cases, reducing ultrasound energy and the amount of time the eye is open
Facility benefits
We are just at the beginning of the learning curve for what we can accomplish with femtosecond lasers in cataract surgery. In the future, new types of IOLs will likely require a precision capsulotomy for proper IOL fixation and accurate centration. As we get smarter about how to actually use all the pre- and intraoperative data the laser obtains, and better able to integrate that data into artificial intelligence algorithms that can identify outliers, I think we are going to see the dawn of a new era in refractive cataract surgery in which surgeons without a laser will be at a significant disadvantage.
For a hospital or surgery center, Investing in a femtosecond laser for cataract surgery is probably very similar to investing in a robotic suite for urologists or general surgeons. Having the femtosecond laser technology makes the facility more attractive to higher volume surgeons who can bring more cases to the operating rooms. This is technology that patients want, surgeons can stand behind, and surgery centers and hospitals should be proud to offer.
References:
- Knobbe CA. Cataract surgery complications. AllAboutVision.com, https://www.allaboutvision.com/conditions/cataract-complications.htm
- Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, et al. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg 2009;35(1):70-5.