Palliative care should be available to anyone with an incurable disease or illness, and it should be provided regardless of age, race, disease, gender or place. Yet, this type of treatment is still not available to a large portion of the population. Many parts of the world, especially those with a low income, still lack a delivery system for palliative care and they don’t have access to the medications needed for palliative care and to treat their pain.
The goal of the World Hospice and Palliative Care Day is to raise awareness and increase the availability of hospice and palliative care throughout the world, in the hope that more people will be able to understand the needs of people living with incurable diseases and provide the much-needed assistance for them and their families.
This year’s theme for the event “Palliative Care – Because I Matter” is a callout to governments to acknowledge the importance of this type of treatment and to listen to the people in need.Everyone matters and should have access to palliative care if they need it.
“You matter because you are you and you matter until the end of your life” – Cicely Saunders.
This year’s World Hospice and Palliative Care Day will be celebrated on Saturday, 13 October and, it is organized by The Worldwide Hospice Palliative Care Alliance. As always, the aim is to:
- Increase the availability of hospice and palliative care throughout the world by creating opportunities to speak out about the issues
- To raise awareness and understanding of the needs of people living with a life-limiting illness and their families
- To raise funds to support and develop hospice and palliative care services throughout the world
Palliative care is a specialized form of medical care specifically designed for people with serious illnesses. The goal is to provide relief from the symptoms and stress related to the illness as well as the procedures and treatment that the patient has to follow. This type of care is appropriate at any age, regardless of the patient’s stage in the illness.
It is known that traditional medical training tends to focus more on the efforts that must be made to cure and prevent the illness, but treating the patient’s symptoms is often overlooked. There are times when all efforts should be focused on looking for a cure at all costs, however, there are times when offering the best care for the patient and his family must become a priority as well and the truth is that the conventional medical training does not provide the necessary tools needed for this type of care.
This is why initiatives like the World Hospice and Palliative Care Day are so important. They raise awareness about a very important topic.
Palliative care does not necessarily mean that you give up on curative treatments and just focus on treating your symptoms in order to achieve the best comfort possible for as long as you’re still alive. Palliative care can be provided while still pursuing and following a curative solution. In fact, many people fully recover during their palliative care treatment and go back to living a fulfilled and joyful life.
If the doctor decides that the patient’s state is not getting any better and that their ongoing treatment is no longer helping, the patient can move from palliative care to hospice care if the doctors estimate that they would die within 6 months. Another possibility is to keep following the curative treatment while increasingly emphasizing comfort care.
Hospice care
During the final stages of a terminal illness, the patient or the patient’s family may discuss with the doctor and decide if the treatment meant to cure or slow the disease are no longer showing any positive progress. When this happens, the doctor may recommend hospice care, also known as end-of-life care.
During hospice care, the aim is to provide the patients with relief from pain and overall improving their quality of life for the remaining time that they have left. Hospice care is not only for the patient himself, but also for their family and the people close to them. It can provide the necessary counseling during these hard times and help them cope with the situation. The hospice care team may include a doctor, nurse, social worker, counselor, chaplain, home health aide, and trained volunteers. This team works together in order to provide the best physical, emotional, and spiritual care for the patient and his loved ones.
Hospice and palliative care for patients affected by mesothelioma and other types of cancer
 One group of people that could benefit greatly from hospice and palliative care are advanced cancer-suffering patients. During their final months, it is important that efforts are made to help them end their days as peacefully as possible, because, in the end, it is the human connection, the ability to feel valuable, significant, to feel like they matter – this is what’s more important for most of the dying patients, not the efforts made to cure the disease, the advanced procedures, or the doctors’ dedication or heroics.
One group of people that could benefit greatly from hospice and palliative care are advanced cancer-suffering patients. During their final months, it is important that efforts are made to help them end their days as peacefully as possible, because, in the end, it is the human connection, the ability to feel valuable, significant, to feel like they matter – this is what’s more important for most of the dying patients, not the efforts made to cure the disease, the advanced procedures, or the doctors’ dedication or heroics.
It is common knowledge that mesothelioma and other asbestos-related types of lung cancer usually responds poorly to treatment and it proves to be fatal in a majority of cases. In these situations, doctors may have a hard time accepting the patient’s wish to stop the curative treatment and they may strongly try to persuade the patient into continuing with the investigations and attempts to cure the disease.
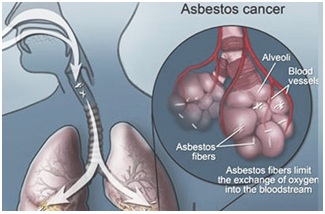 It’s understandable that a doctor really wants the treatments they recommended to work, and so is their frustration when they don’t, however, in the end, it is important to remember and listen hard to the patient’s needs and desires, to give them the straight truth, and overall provide assistance with the decisions that are right for them.
It’s understandable that a doctor really wants the treatments they recommended to work, and so is their frustration when they don’t, however, in the end, it is important to remember and listen hard to the patient’s needs and desires, to give them the straight truth, and overall provide assistance with the decisions that are right for them.
This is where palliative care steps in – when the patient’s outcome is clear, palliative care can help create a situation that maintains and improves the quality of life for the dying patient.




















