When trying to figure out what ‘best’ to do for the UK and globally in these unprecedented times, it is easy to become paralysed with indecision at the options. Do we prioritise the NHS while keeping the economy closed and people at home, or is it ‘best’ to open the economy and try to save jobs, knowingly increasing pressure on healthcare workers?
Add to this the threat of a ‘twindemic’ with seasonal flu and that indecision deepens. The biggest challenge is people. People spread the pandemic, the pathogens, and the possibility of more problems, and no amount of cleaning, face masks, or hand sanitising can fully eliminate risk as long as people keep interacting. So, what should we do?
Air sterilisation might just be the unsung hero for this problem, both within and beyond the healthcare setting, and both as a short-and long-term solution to support the economy reopening without deepening the risk.
How long will people be prepared to wear masks in public or stick with the rule of six? Shouldn’t we be looking ahead to see how we create long-term pathogen controls in public places and offices, not only to reduce the immediate risk and deliver infection control, but also to generally decrease infection risk and absenteeism within the economy?
This can then go hand in hand with the longer-term proactive measures like vaccine and medicine developments which will no doubt help to reduce and treat cases, minimising deaths in the coming years.
What is air sterilisation and how does it help?
Aside from the emergence of new, unseen pathogens like Covid-19, the biggest challenge in infection control stakes is the movement of people. An area is only ‘clean’ in the moments after it has been cleaned, before people make their way through it; coughing, spluttering, and touching, when aerosolised spores and pathogens start to resettle on surfaces.
Add to this the long-tail incubation period of Covid-19 and a single infected individual is unknowingly spreading the virus for days before they show any symptoms.
Current guidance for managing infection risk has three core focuses: cleaning, accurate record-keeping, and space adaptations such as Perspex screens. The question is whether these steps are enough, or whether they just create the perception of safety within an environment.
According to research by King’s College London, who ran an antibody testing study, at least one in five people from the group didn’t show any symptoms at all of Covid-19 despite having, or having had the virus. Meanwhile more than 25 per cent who did fall ill, did so without having any of the three core symptoms that commonly identify those with Covid-19. The average business cannot claim to be infection control experts, so how can we manage the real risk of infection effectively?
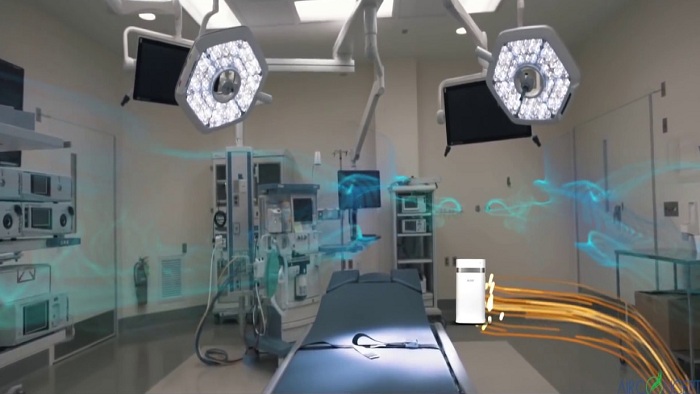
Air sterilisation is not actually a new solution, but it is in my opinion a severely underutilised one. It involves the installation of a discrete, standalone unit which works by using a series of air and surface purification technologies to help manage infection risk in a room.
Each brand varies slightly in terms of what techniques are used and how effective they are, but they will have a set purpose to neutralise microbes, bacteria, dust or even odours. We are the UK distributors for a brand called AIRsteril for example, which works both for air sterilisation and surface sterilisation by producing plasma quatro.
The AIRsteril technology specifically combines sterilising, cleaning, and purifying technologies, including germicidal UV light, dual UV operation, Photocatalytic Oxidation (PCO) and a purifying plasma of superoxide ions and optimal ozone. These techniques together kill up to 99.9 per cent of germs and viruses, before releasing the purified air back into the room as a plasma.
The plasma then kills airborne pathogens, viruses, bacteria, fungi, mould spores and allergens, and decomposes odours and harmful gases. Its effectiveness was tested by Leeds University and shows that airborne microorganisms were undetectable after just 60 minutes.
This is where things get really cool, as the process not only manages airborne infection risk, but also sanitises surfaces and the wider environment. The purified plasma breaks down microorganism cell walls, destroying the cells and preventing them from reproducing. As the plasma moves over surfaces – any surfaces including hard and soft materials – it also kills the germs which are left behind by touching, breathing and coughing or which have settled in the environment.
The core advantage is that it works constantly, so even if people move around and leave pathogens behind in between cleaning schedules, viruses and bacteria will likely be eliminated in a matter of minutes if not hours. To put this into context, AIRsteril was tested in a quantified NHS call centre environment, prior to the pandemic; constant air sterilisation resulted in a 42 per cent reduction in absenteeism, particularly for asthma, cold, cough, influenza, chest, and respiratory problems.
While the priority here was managing absenteeism, this model translates to significantly reduced infection transfer, and significantly reduced disruption through suspected Covid-19 cases.
For me, the solution isn’t simple, but I genuinely believe that we can successfully minimise infection risk through a combined effort of public and private measures, medicine and vaccines, and with the addition of active technologies like air sterilisation to manage the overall risk.