The Impact of AI-Driven Clinical Decision Support Systems on Hospital Efficiency and Patient Safety
Transforming Healthcare Through Intelligent Technology
The integration of artificial intelligence into clinical decision support systems represents one of the most significant technological advances in modern healthcare. As hospitals worldwide grapple with increasing patient volumes, rising costs, and growing demands for improved outcomes, AI-driven Clinical Decision Support Systems (AI-CDSS) have emerged as powerful solutions that simultaneously enhance operational efficiency and patient safety outcomes.
The global clinical decision support systems market, valued at USD 5.79 billion in 2024, is projected to reach USD 10.71 billion by 2030, reflecting the growing recognition of these technologies’ transformative potential. This remarkable growth trajectory underscores healthcare organizations’ increasing confidence in AI-powered solutions to address critical operational challenges while maintaining the highest standards of patient care.
Redefining Clinical Excellence Through AI Integration
The modern healthcare landscape demands precision, speed, and consistency in clinical decision-making. Traditional decision support systems, while valuable, often fall short in processing the vast amounts of complex data generated in contemporary medical practice. AI-driven systems bridge this gap by leveraging machine learning algorithms, natural language processing, and deep learning models to analyze patient data with unprecedented accuracy and speed.
Recent implementation studies demonstrate remarkable improvements across multiple performance metrics. Diagnostic accuracy has increased from the traditional 75-80% baseline to an impressive 87-92% with AI assistance. This enhancement represents more than statistical improvement; it translates directly into better patient outcomes, reduced misdiagnoses, and more targeted treatment interventions.
The sophistication of these systems extends beyond simple diagnostic support. AI-CDSS platforms now provide real-time risk stratification, personalized treatment recommendations, and predictive analytics that enable healthcare providers to intervene before adverse events occur. For instance, advanced deep learning models have demonstrated the ability to predict cardiovascular events in diabetic patients with remarkable precision, enabling proactive interventions that prevent serious complications.
Operational Efficiency and Cost Optimization
Streamlining Administrative Processes
One of the most immediate and measurable impacts of AI-CDSS implementation lies in administrative efficiency improvements. Healthcare systems implementing these technologies report administrative time savings ranging from 25% to 50%. These improvements stem from the automation of routine tasks such as clinical documentation, prescription verification, and patient data processing.
The economic implications are substantial. Administrative costs, which typically account for 15-30% of total healthcare expenditures, can be significantly reduced through AI automation. McKinsey analysis suggests that AI-enabled prior authorization processes alone could decrease manual effort by 50-75%, freeing healthcare professionals to focus on direct patient care activities.
Natural language processing capabilities within AI-CDSS have revolutionized clinical documentation workflows. Systems can now automatically extract relevant information from unstructured clinical notes and populate electronic health records with structured data, reducing documentation time by an average of 7.8 minutes per patient encounter. This efficiency gain accumulates to significant time savings over the course of a typical clinical day.
Resource Allocation and Workflow Optimization
AI-driven systems excel at optimizing resource allocation through predictive analytics and real-time monitoring. Hospitals implementing these technologies report improvements in patient flow management, with average length of stay reductions of approximately 19.4%. This improvement results from more accurate discharge planning, better coordination of care transitions, and proactive identification of patients ready for discharge.
The systems’ ability to predict patient acuity and resource needs enables more effective staffing decisions and equipment allocation. Predictive models can analyze historical data, seasonal patterns, and current patient census to forecast demand, allowing administrators to deploy resources more strategically. This optimization reduces both operational costs and patient wait times while ensuring adequate staffing levels during peak demand periods.
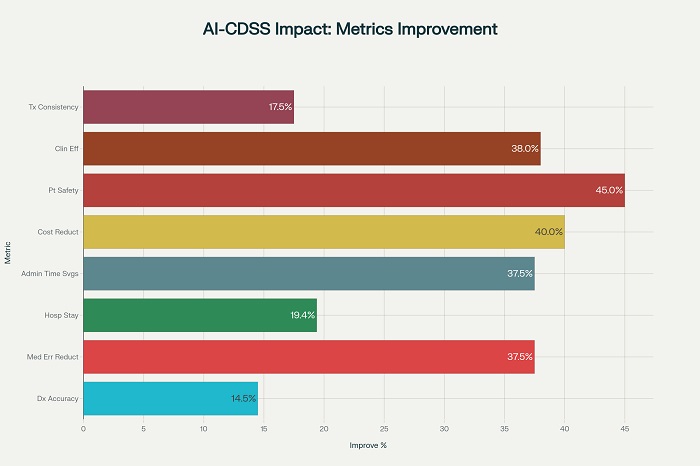
Key performance improvements achieved through AI-driven clinical decision support systems implementation
Patient Safety Enhancement Through AI Intelligence
Medication Error Prevention
Medication errors represent a significant patient safety concern, with traditional rates ranging from 15-20 errors per 100 admissions. AI-CDSS implementation has demonstrated the ability to reduce these rates to 8-12 errors per 100 admissions, representing a 35-40% improvement in medication safety. These systems provide real-time alerts for drug interactions, dosage errors, and contraindications, creating multiple safety checkpoints throughout the medication administration process.
The financial impact of medication error prevention extends beyond immediate safety benefits. Preventable medical errors cost the healthcare system approximately $20 billion annually, making error reduction a critical component of cost containment strategies. AI systems contribute to this reduction through continuous monitoring of prescribing patterns, patient responses, and potential adverse reactions.
Predictive Risk Assessment
Advanced AI algorithms excel at identifying patients at high risk for adverse events before clinical deterioration becomes apparent. These systems analyze multiple data streams including vital signs, laboratory values, medication histories, and clinical notes to generate risk scores that guide clinical interventions. Early warning systems for conditions such as sepsis, falls, and cardiac events have shown remarkable success in preventing serious complications.
The implementation of AI-powered sepsis detection systems has yielded particularly impressive results. Johns Hopkins Medicine reported up to 20% reductions in ICU mortality following deployment of AI-based early sepsis detection tools. Similar improvements have been documented for fall prevention, pressure ulcer avoidance, and postoperative complication reduction.
Quality Assurance and Clinical Consistency
AI-CDSS contributes significantly to clinical quality assurance by promoting evidence-based decision-making and reducing practice variation. Treatment consistency rates have improved from baseline levels of 70-75% to 85-90% following system implementation. This improvement reflects the systems’ ability to provide standardized, guideline-based recommendations that reduce subjective variability in clinical decision-making.
The systems also enhance quality monitoring through automated documentation review and outcome tracking. AI algorithms can identify patterns in clinical data that might indicate quality issues, enabling proactive interventions before problems become systemic. This capability is particularly valuable in complex clinical environments where manual monitoring of all quality indicators would be resource-prohibitive.
Economic Impact and Return on Investment
Financial Analysis and Cost-Benefit Considerations
The economic justification for AI-CDSS implementation requires careful analysis of both direct and indirect costs and benefits. Initial implementation costs typically range from $725,000 to $1.2 million for comprehensive systems, with annual maintenance costs of approximately $185,000. However, the return on investment becomes apparent relatively quickly, with most organizations achieving positive ROI within 2-3 years of implementation.
Annual cost savings from AI-CDSS implementation average $2.75 million for large healthcare systems. These savings derive from multiple sources including reduced medication errors ($850,000 annually), shortened length of stay ($1.2 million annually), administrative efficiency gains ($400,000 annually), and reduced readmissions ($300,000 annually).
The five-year net ROI for comprehensive AI-CDSS implementation typically exceeds $11 million when accounting for all direct and indirect benefits. This substantial return reflects not only cost savings but also revenue enhancement through improved patient throughput, reduced liability exposure, and enhanced reputation for quality care.
Value-Based Care Alignment
AI-CDSS implementation aligns particularly well with value-based care initiatives that emphasize outcomes over volume. These systems support value-based care goals by tracking and improving key performance metrics such as readmission rates, preventive care delivery, and patient satisfaction scores. The ability to demonstrate measurable improvements in these areas positions healthcare organizations favorably for value-based contracts and quality incentive programs.
The systems’ predictive capabilities enable proactive care management that reduces expensive acute care episodes. By identifying high-risk patients early and facilitating appropriate interventions, AI-CDSS helps shift care delivery from reactive treatment to preventive management, aligning with the fundamental principles of value-based healthcare.
Implementation Challenges and Strategic Solutions
Technical and Organizational Barriers
Despite the clear benefits, AI-CDSS implementation faces significant challenges that organizations must address strategically. Technical barriers include data integration complexities, system interoperability issues, and concerns about algorithm transparency. Many healthcare organizations operate with legacy systems that were not designed for AI integration, requiring substantial infrastructure investments and technical expertise.
Organizational barriers often prove more challenging than technical issues. Workflow integration requires careful analysis of existing processes and gradual implementation to minimize disruption. Change management becomes critical, as clinical staff must adapt to new decision-making processes while maintaining confidence in their clinical judgment. Training requirements are substantial, requiring ongoing education programs to ensure effective system utilization.
User Acceptance and Trust Building
Healthcare professionals’ acceptance of AI-CDSS depends heavily on system design, transparency, and demonstrated value. Automation bias represents a significant concern, where clinicians may become overly reliant on system recommendations without appropriate clinical judgment. Conversely, some practitioners may resist AI recommendations due to concerns about professional autonomy or system reliability.
Successful implementation requires user-centered design approaches that involve clinical staff in system development and refinement. Transparency in algorithm decision-making, clear explanations of recommendations, and easy override mechanisms help build trust and appropriate utilization patterns. Regular feedback collection and system updates based on user experience contribute to long-term acceptance and effectiveness.
Regulatory and Compliance Considerations
The regulatory landscape for AI in healthcare continues to evolve, creating uncertainty for organizations considering implementation. Approval and certification processes for AI-enabled medical devices can be complex and time-consuming, with limited numbers of qualified certifying bodies creating bottlenecks. Data privacy compliance, particularly under regulations such as GDPR, requires careful attention to data handling, storage, and access controls.
Healthcare organizations must develop comprehensive governance frameworks that address these regulatory requirements while enabling innovation. Privacy-by-design approaches, regulatory consultation during development, and robust audit trails help ensure compliance while supporting system effectiveness.
Future Directions and Emerging Opportunities
The evolution of AI-CDSS continues to accelerate, with emerging technologies promising even greater impact on hospital efficiency and patient safety. Integration with Internet of Things devices, wearable sensors, and remote monitoring systems will expand the data available for clinical decision-making while enabling more continuous patient monitoring.
Blockchain technology integration offers potential solutions to data security and interoperability challenges, while advances in explainable AI will address current concerns about algorithm transparency. The development of more sophisticated natural language processing capabilities will further enhance documentation efficiency and clinical communication.
The growing emphasis on personalized medicine creates new opportunities for AI-CDSS to provide more targeted, patient-specific recommendations. Integration with genomic data, lifestyle factors, and social determinants of health will enable more comprehensive risk assessment and treatment optimization.
Maximizing Implementation Success
Healthcare organizations pursuing AI-CDSS implementation should adopt a strategic, phased approach that addresses both technical and human factors. Initial implementation should focus on high-impact, low-risk applications that demonstrate clear value while building organizational confidence and expertise. Comprehensive training programs, ongoing support, and regular performance monitoring are essential for sustained success.
Collaboration between clinical, technical, and administrative stakeholders ensures that system design meets real-world operational needs while addressing practical implementation challenges. Regular assessment of outcomes, user satisfaction, and system performance enables continuous improvement and optimization of the investment.
The evidence clearly demonstrates that AI-driven clinical decision support systems represent a transformative opportunity for healthcare organizations. When implemented thoughtfully with attention to both technical requirements and human factors, these systems deliver substantial improvements in hospital efficiency and patient safety while providing strong economic returns. As the technology continues to evolve and mature, the potential for even greater impact on healthcare delivery becomes increasingly evident, positioning AI-CDSS as an essential component of modern healthcare infrastructure.
















