Key Takeaways
- Digital health tools increase medication adherence by 25-40% through intelligent reminder systems and patient education features
- Personalized health feedback platforms improve patient engagement scores by 50% or more, driving better clinical outcomes
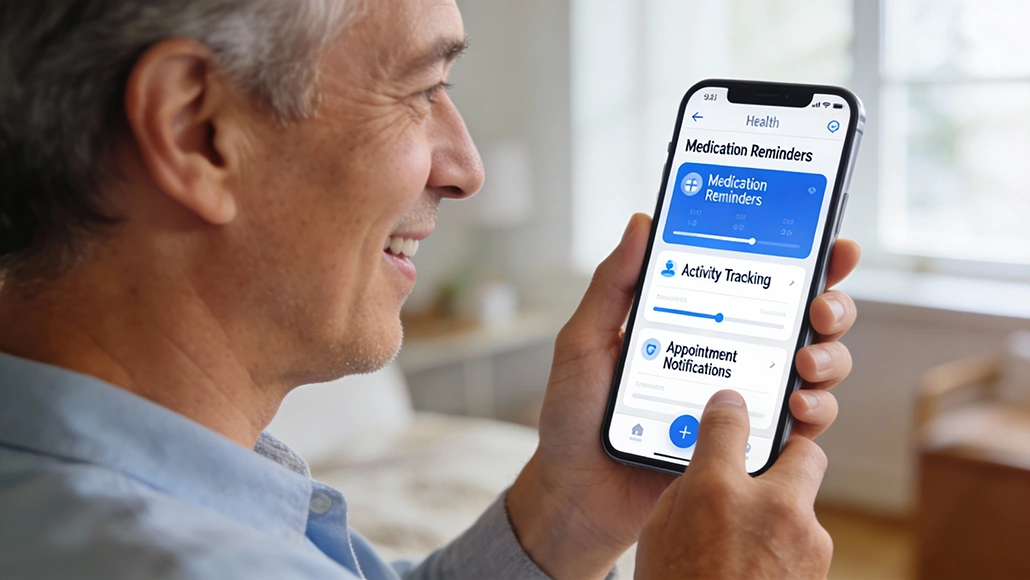
- Mobile health applications reduce no-show rates for appointments by 30-35% through automated reminders and scheduling features
- Real-time health tracking through digital platforms enables early identification of clinical deterioration, supporting timely interventions
- Patient portals and secure messaging systems increase care coordination efficiency and patient satisfaction simultaneously
- Gamification and social engagement features in digital health tools increase long-term wellness behavior adoption by 45-55%
Patient engagement represents one of healthcare’s most persistent challenges. Despite advances in treatment options, medications go untaken, appointments are missed, and lifestyle modifications remain unachieved. Studies consistently demonstrate that patient behavior medication adherence, lifestyle choices, engagement with healthcare providers drives clinical outcomes at least as significantly as the underlying treatment itself. Digital health technology offers unprecedented opportunities to address this engagement gap. Digital patient engagement tools are fundamentally reshaping how healthcare organizations connect with patients, moving from passive information recipients to active participants in their own health management.
The Foundation: Understanding Patient Engagement Barriers
Before exploring digital solutions, it’s crucial to understand why patient engagement fails. The barriers are multifaceted. Patients often lack understanding of their conditions and why recommended treatments matter. Busy lives make it easy to forget medications or appointments. Some experience “treatment fatigue” the psychological burden of managing chronic conditions. Others lack confidence that their efforts will produce meaningful results. Healthcare systems, designed around provider convenience rather than patient experience, create additional friction.
Digital patient engagement tools address these barriers systematically. Rather than assuming patients will remember to take medications or maintain lifestyle changes, digital platforms provide persistent reminders and continuous support. Rather than expecting patients to understand complex disease mechanisms, these tools translate medical information into accessible, personalized insights. Rather than waiting for patients to self-report problems, digital systems enable continuous monitoring and early detection of emerging issues.
Personalized Feedback Systems Driving Behavioral Change
One of the most powerful features of modern digital patient engagement tools involves personalized health feedback. Rather than generic advice applicable to populations, these systems provide feedback tailored to individual circumstances. A patient with hypertension receives different guidance than one with diabetes, and both receive different advice than a healthy person focused on prevention.
Modern health platforms integrate multiple data sources patient demographics, medical history, current health metrics from wearable devices, medication lists, lab results to generate truly personalized recommendations. Machine learning algorithms identify patterns in patient data, predicting which behaviors will have the greatest impact for that specific individual. For a sedentary diabetic patient, increasing physical activity might have greater blood sugar impact than dietary modification; the system prioritizes exercise support. For another patient, dietary changes prove more impactful; the system emphasizes nutrition guidance.
This personalization extends to communication style and timing. Some patients respond to frequent detailed information; others prefer brief, occasional messages. Digital platforms increasingly use machine learning to identify individual preferences, then adapt their engagement approach accordingly. A patient might receive weekly detailed health summaries while another receives brief daily motivation messages. Engagement increases when communication matches individual preferences.
Intelligent Reminder Systems and Medication Adherence
Medication non-adherence costs the healthcare system an estimated $290 billion annually in preventable medical spending. Patients forget doses, discontinue medications when feeling better, or struggle with complex regimens involving multiple drugs at different times. Digital patient engagement tools address these challenges directly.
Medication reminder systems vary in sophistication. Basic approaches send notifications at medication times, simply reminding patients to take doses. More advanced systems understand medication complexity, recognizing that some drugs must be taken with food while others require empty stomachs. The system provides contextual reminders tailored to these requirements.
Intelligent reminders progress further, understanding that simple notifications often prove insufficient for chronic adherence. Some systems employ behavioral psychology principles, using messages emphasizing benefits of medication adherence or potential consequences of non-adherence. Others use motivational language, praising successful adherence streaks or offering encouragement during challenging periods. Gamification elements earning points for consistent adherence, unlocking badges, competing with friends add engagement layers that increase long-term medication taking.
Data demonstrates substantial impact. Patients using structured reminder systems show 25-40% improvements in medication adherence compared to those without support. This improvement translates directly to better blood pressure control, improved cholesterol levels, reduced hospital readmissions, and lower overall healthcare costs.
Real-Time Health Monitoring and Preventive Intervention
Traditional healthcare operates reactively patients develop symptoms, contact providers, and receive treatment. Digital patient engagement tools increasingly enable proactive care, where continuous monitoring identifies problems before symptom development.
Wearable devices integrated with digital health platforms provide continuous data streams on vital signs, activity levels, sleep quality, and other health indicators. Machine learning algorithms analyze these streams, identifying subtle changes that might indicate emerging health problems. A patient’s normal heart rate pattern might be 60-70 beats per minute; when sustained elevation to 85-90 appears, the system alerts the patient and healthcare provider. This early warning enables intervention before symptoms become severe.
Real-time monitoring proves particularly valuable for high-risk populations. Patients with heart failure benefit from weight monitoring a 2-3 pound weight gain over 24 hours might indicate fluid accumulation requiring clinical attention. Digital systems can alert patients and providers to this concerning change within hours rather than waiting for a scheduled appointment weeks away. Studies demonstrate that remote monitoring combined with early intervention reduces heart failure hospitalizations by 25-30%.
Patient Portals and Care Coordination
Secure patient portals represent foundational digital patient engagement tools, providing patients with access to medical records, test results, medication lists, and appointment scheduling. Patients no longer passively wait for provider communication; they can actively monitor their care and health information.
Portal effectiveness increases substantially when combined with provider engagement. Portals enabling secure messaging between patients and providers improve care coordination efficiency. A patient can ask medication questions without scheduling an appointment; providers respond asynchronously, reducing unnecessary office visits. Patients can report emerging symptoms; providers assess urgency and guide appropriate response. Lab results appear in patient portals with interpretation aids, helping patients understand results in context.
Importantly, patient portals increase healthcare transparency and patient satisfaction. When patients can see their medical records, they develop greater understanding of their conditions and treatments. Medication errors are reduced as patients identify discrepancies between prescribed and documented medications. Provider recommendations carry greater weight when patients understand the reasoning behind them.
Health Education and Patient Empowerment
Knowledge represents a critical foundation for engagement. Patients who understand their conditions and why treatments matter demonstrate greater engagement and better outcomes. Digital patient engagement tools provide unprecedented opportunities for scalable patient education.
Rather than limiting education to office visits where time is constrained, digital platforms offer continuous learning opportunities. Interactive educational modules explain disease mechanisms, treatment options, and lifestyle modifications. Videos demonstrate proper medication administration or exercise techniques. Quizzes assess understanding and identify knowledge gaps for targeted reinforcement. All this education is accessible when convenient for patients evenings, weekends, whenever they choose rather than during office hours.
Importantly, effective patient education empowers patients to become active healthcare participants rather than passive recipients. A patient understanding how medications work, why lifestyle changes matter, and what warning signs warrant urgent care is far more likely to engage effectively in their treatment. This empowerment addresses one of the deepest engagement barriers the sense of helplessness that often accompanies chronic illness.
Behavioral Modification and Lifestyle Change Support
While medications address disease biology directly, many conditions require behavioral changes for true control. Hypertension requires dietary sodium reduction and increased exercise. Diabetes requires dietary modification and activity increases. These behavior changes prove difficult, often requiring sustained effort over years.
Digital patient engagement tools support behavioral change through multiple mechanisms. Goal-setting features help patients define specific, measurable objectives. Progress tracking shows whether efforts are working, providing motivation through visible improvement. Social engagement features enable patients to share experiences, offer mutual support, and celebrate successes together. Some platforms connect patients with behavioral coaches who provide personalized guidance.
Motivational interventions, drawn from psychological research, increase the likelihood of successful behavior change. Rather than simply telling patients to exercise, effective platforms help patients identify personally meaningful reasons for change, remove barriers to implementation, and support persistence through inevitable setbacks. A patient who exercises because they want to see their grandchildren grow up demonstrates different motivation and likely better adherence than one who exercises because a doctor said to.
Integration with Healthcare Providers
The most effective digital patient engagement tools exist within integrated ecosystems where patient-generated data informs provider decision-making. Rather than providers and patients operating independently, digital platforms facilitate true collaboration.
Providers accessing patient-generated data through secure platforms gain insights into patients’ daily lives between office visits. Blood pressure readings over 30 days provide far richer information than the single office reading. Activity patterns, sleep quality, and symptom reporting create comprehensive pictures of patient experience. This information enables providers to make more informed treatment decisions adjusting medications based on actual data rather than guesses, identifying lifestyle barriers to health, and providing targeted interventions.
Notably, this integration increases patient trust in providers. When providers demonstrate awareness of patient challenges, acknowledge progress made, and provide evidence-informed guidance, patients feel heard and supported. This therapeutic alliance the relationship between patient and provider independently improves health outcomes beyond what any individual intervention achieves.
Overcoming Adoption and Equity Challenges
Despite potential benefits, digital health adoption remains uneven. Older adults, those with limited digital literacy, and socioeconomically disadvantaged populations face barriers to engaging with technology-based platforms. Successful digital patient engagement tools must address these equity considerations.
User interface design significantly impacts adoption. Overly complex systems requiring substantial technological sophistication exclude vulnerable populations. Intuitive, simple interfaces increase adoption across demographic groups. Offering multiple engagement pathways website portals, mobile apps, phone-based systems accommodates individual preferences and technological access.
Language accessibility represents another critical consideration. Patients should engage with platforms in their preferred language. This requires substantial translation and cultural adaptation efforts, ensuring guidance is appropriate across diverse backgrounds. Provider training in digital platform usage ensures they can effectively integrate patient-generated data into decision-making.
The Future: AI-Enhanced Personalization and Predictive Analytics
The trajectory of digital patient engagement tools points toward increasingly sophisticated AI integration. Rather than reactive engagement responding to patient-reported data, next-generation systems will use predictive analytics to anticipate patient needs.
Machine learning models analyzing longitudinal patient data will identify individuals at risk of non-adherence, clinical deterioration, or treatment failure before these problems manifest. Systems will then trigger proactive interventions intensified support for patients showing non-adherence risk, earlier consultations for those showing subtle deterioration signs. This shift from reactive to predictive engagement will enable genuinely preventive healthcare.